Deep infiltrating endometriosis.
Hi, This is my first ever written article, and it’s about my wife who developed stage IV endometriosis, deeply infiltrating endometriosis, or “DIE” for short, so please, bear with me.
Some of you may be asking endo what? Never heard of it! Others on the other hand may be familiar with this awful illness causing pelvic pain caused by scar tissue, which estimated prevalence is that it actually affects 10% of the female population worldwide reducing their quality of life, but is extremely difficult to diagnose.
The struggle that women go through trying to get a diagnosis for this condition often results in them suffering mental health problems, as was the case for my wife. There are lots of other medical conditions that affect mental health, especially if they are causing you to have a low quality of life, but in this article, I am focusing on one very close to my heart, as it has affected my wife.
Also, both I and my wife are trying to bring awareness to people regarding deep infiltrating endometriosis as it is a very difficult disease to get diagnosed despite distinguishing pelvic pain and there is currently no cure for it!
Today, my wife, I will call her M as she would like to keep her identity private for the time being, is 3.5 weeks into her recovery from laparoscopic surgery for stage IV deeply infiltrating endometriosis.
She went under general anaesthetic as a day case for a diagnostic laparoscopy to determine whether she had endometriosis or not, but the surgery was extended to 3.5 hours as they did find quite extensive endometriosis scar tissue, which was everywhere including her bowel and bladder endometriosis.
M has put together the rest of this article explaining a little bit about her struggles with the disease and the all-important facts regarding theories for the cause of the disease, diagnosis and treatment, and the effects that it has on mental health. So please read on…
M’s words about her DIE…
Endometriosis is a chronic illness that destroys the lives of many women. The suffering of chronic pelvic pain is hard to deal with and diagnosis takes 7 to 8 years in the UK and even longer in other countries. It affects 1 in 10 women. Yes, it’s really that common!
Its impact on a woman’s life is sometimes devastating and it has tried to invade our marriage, but we don’t let it beat us and ruin our lives. This article is aimed at educating people on what deeply infiltrating endometriosis is, what the current treatments are, and the effects that it has on sufferers and their partners.
In my case, the symptoms of pelvic pain caused by endo and scar tissue started to become more and more severe about 5 years ago, although the surgeon that removed my endometriosis expected that I had probably had the disease way longer than that. My bladder endometriosis made me constantly pee.
I have always suffered from anxiety and depression since my teenage years, due to certain life events that I won’t go into in this particular article.
I was on Prozac from the age of 18 until 35 when finally came off them by tapering the dose over a long period of time. This was because I got married to my lovely husband, we wanted to have a baby, and taking antidepressants whilst pregnant is not recommended due to the possibility of harm to the foetus.
When I was around the age of 38/39, I started to get my first symptoms of deeply infiltrating endometriosis:
- heavy bleeding (flooding my clothes)
- severe back and side pain
- chronic pelvic pain caused by scar tissue
- severe menstrual cramps
- problems with my digestion
- bladder endometriosis (pee a lot)
I had previously been a dance teacher/performer, I was going to the gym on a regular basis and also had a part-time job as a medical secretary for the NHS. Some would say that I was super fit, however, over the following 5 years, my health deteriorated year after year.
The beginning…
First, I started to suffer from severe pelvic pain and back pain which forced me to give up dancing and teaching professionally, and that in itself was the worst thing that could happen to me as it was something I had been doing for a lifetime and something that I truly loved.
I then became anaemic due to heavy periods, and then it seemed like anything I ate gave me digestive problems. I couldn’t take iron tablets as they made me so sick, so it was suggested that I try the combined contraceptive pill or the progesterone-only pill to try and stop the heavy bleeding.
Unfortunately, these were not options for me as I had previously come off the combined pill due to bad migraines and as I was over 35 and had a history of stroke in the family I was advised not to take these and try the progesterone-only pill, which still gave me headaches on top of mood swings, brain fog and it didn’t stop the bleeding.
I kept going to work suffering through the pain, sometimes having to call at the last minute and take time off due to the heavy bleeding and pelvic pain I was suffering. I also needed to pee a lot due to my bladder endometriosis.
I felt so guilty and terrible every time this happened and was always worried about the workload I would have to get through when I went back to work.
I then started to suffer from severe anxiety and panic attacks which resulted in me being taken to A&E on multiple occasions.
I made countless visits to the GP who basically thought that my symptoms were all stress-related, and since I did have a stressful job working for the NHS and had previously suffered from anxiety and depression, I started to believe that this was possible.
They offered me antidepressants and counselling, but I declined the antidepressants and went for counselling.
The digestive problems.
In February 2018 I was referred to gynaecology for further investigation as the bleeding had gotten even heavier, my digestive symptoms were worse, and I had lost 5kg in weight in a few months.
I had an investigation called a hysteroscopy to look inside my womb, and they found polyps that were removed; otherwise, they said everything was normal including ultrasound, and this reassured me that the heavy bleeding and pain were due to the polyps.
They suggested that the polyps were probably caused by a hormone imbalance and the rest of the symptoms were probably due to perimenopause.
In September 2018 I was at work and started to have really bad pelvic pain and feel sick. I carried on with my work trying to ignore it and before I left realised that I had come on my period.
I hadn’t managed to get home before I had started to flood my clothes again and I had to jump in the shower and let the blood just gushing out of me. I put some very thick sanitary pads on doubled up and went upstairs to lay down in my room, but when I stood up to use the toilet the blood just gushed out everywhere, all over the floor!
My mum and dad had to get towels for me to hold against myself to stop the bleeding and I started to pass out! I was admitted to the hospital by ambulance, they stabilised me and gave me some drugs to stop the bleeding but suggested that I go back to my GP to order an urgent scan.
My GP did not arrange the urgent scan, as he said that I had had a hysteroscopy and nothing new would be there within a few months. Instead, he suggested that it was all probably due to hormonal changes. He referred me to a specialist clinic for severe PMS as I was exhibiting all the symptoms, including pelvic pain.
The diagnosis.
I was seen in the Menopause/PMS clinic in November 2018 and they immediately arranged bloods and an urgent scan which finally revealed an endometrioma on my right ovary (a cyst associated with stage 4, in my case deeply infiltrating endometriosis) thankfully they referred me to a pelvic pain specialist Endometriosis Clinic.
An MRI was arranged to see if I had any more endometriosis lesions in my pelvis, but nothing showed up apart from the endometrioma (cyst). I did my research and realised that for lots of women the extent of the deeply infiltrating endometriosis had not shown up on a scan, so I pushed for a laparoscopy (the gold standard of treatment).
I waited until August 2019 before I finally had the laparoscopy by a specialist surgeon to diagnose the deep infiltrating endometriosis and treat it, but at least I have peace of mind now that all those years I was suffering from this invisible disease and it wasn’t all in my head!
Naturally, my husband noticed my struggles with my invisible illness. The pain was excruciating but I did not know how to show it to my family, friends, and even doctors who didn’t believe me.
I helped my husband write an e-Book about endometriosis. “Endo-Tool, Endometriosis for Men” e-Book’s FREE 1st chapter gives you 20 pages filled with pure value, such as:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types? (i.e. bladder endometriosis)
- What is adenomyosis and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”!
an Endometriosis for Men book

DIE, the facts!
Since this article is quite a long one, to make it easier for you to navigate through it, I have decided to dissect it into a few segments. The table of contents will allow you to skip between each section.
It is advisable to go from the first point to the last to get a sense of it all, but feel free to jump to any section you want. In this article you will find:
- Endometriosis the disorder
- Early symptoms of Endometriosis
- Current theories on the cause of Deep Infiltrating Endo
- Diagnosis
- Treatment options
- Nutrition & Alternative Therapies
- Fertility
- Endometriosis Support Groups
- How Endometriosis affects couples
1. DIE.
Endometriosis is a condition whereby tissue similar to the lining of the womb (endometrium-like tissue, called endometriotic lesions) somehow implants outside the womb. Endometriotic lesions (scar tissue), which are like blisters can be found anywhere in the pelvic cavity.
They can be found on the ovaries, fallopian tubes, the uterosacral ligaments, and the pouch of Douglas (situated behind the womb), and also on other organs in the pelvic cavity such as the bladder endometriosis, and the bowel, intestines, colon, appendix, and rectum.
These lesions bleed every month when a woman has her period with the fluctuation of hormones, just as the lining of the womb sheds, and when they bleed, they can implant and spread to another location.
Deep infiltrating endometriosis can cause scar tissue (adhesions), which can make internal tissues sticky and sometimes cause internal organs to fuse together. Endometriosis causes severe pain and can also cause infertility and other complications.
Having endometriosis is like having tens or hundreds of excruciatingly painful blisters or bee stings covering the inside of your pelvis (pelvic pain). Deep infiltrating endometriosis can affect women of any age but it’s most common in women in their 30’s and 40’s. I was diagnosed at the age of 44.
It usually takes 7 to 8 years, so I got quite lucky to be diagnosed after 5 years of quite severe symptoms.
Endometriosis is a chronic and life-lasting condition. There are ways to treat the symptoms of endometriosis, with hormones and/or surgery or both. However, there is no cure for it and even after specialist excision surgery, there is still a risk of it coming back at a later stage. Endometriosis affects 10% of the female population.

The symptoms that women suffer from deep infiltrating endometriosis can also have a devastating effect on their mental health and cause them to feel anxious, depressed, and sometimes even suicidal.
If you or your loved one are suffering from this disease, our hearts go out to you, as we truly understand the struggles that you are facing.
We are going to try and give as much information on the subject as possible and help you will ways to cope, so you or your partner don’t have to go through the same struggles we’ve been through trying to find answers.
We are also trying to bring awareness to people regarding this awful condition in the hope that more research can be done for a cure.
2. Early symptoms of deeply infiltrating endometriosis.
Let’s talk about symptoms and the early stages of deep endometriosis because women can start suffering from it as early as their teenage years can suffer from it. Catching it before its advanced stages with plenty of lesions and scar tissue, it is important as not only does it cause years of pain and misery, but it can damage a women’s anatomy and may also render her infertile.
Symptoms of endometriosis are as follows, but they don’t all always happen together at the same time, until maybe in the later stages of the disease, this is why deep infiltrating endo is so hard to diagnose:
- Really long or extremely heavy periods
- Pelvic pain caused by scar tissue
- Severe migraines
- Severe lower back, pelvic, and sometimes leg pain during your period
- Painful bowel movements
- Peeing a lot (bladder endometriosis or urinary tract endometriosis)
- Allergies that get worse around your period
- Bleeding between periods
- Fatigue
- Nausea
- Diarrhoea
- Pain on intercourse
Normal menstrual cramps can usually be relieved with over-the-counter medication or home remedies such as hot water bottles, which help to reduce the pain. But the cramps from endometriosis are sometimes called “killer cramps” because they can be so severe, that they stop you in your tracks.
Deep infiltrating endometriosis pain can feel so intense, it can affect your daily routine and it can even stop you from doing some of the things you love. On a bad day, I couldn’t do basic tasks as I couldn’t focus on anything but the pain, and over-the-counter painkillers aren’t always helpful enough.
For a lot of women, the condition gets worse as they get older but dealing with symptoms eases the pain. Other kinds of pain you can experience can be misleading and thought of as unrelated, but they could be symptoms of endometriosis.
Pelvic pain and belly pain might start before your period and last for several days and it can also happen during ovulation. It can feel sharp or stabbing and it usually won’t go away.
Some women say it feels like their insides are being squeezed or pulled around, and they have a gnawing or throbbing feeling that can be severe.
Nerve and muscular pain can be felt in the legs, lower and upper back, pelvic pain, and some women even complain of shoulder pain. The most common symptoms are the following:
- Backache and pelvic pain are common because your uterus and ovaries are near your back.
- Leg pain, because endometriosis can affect nerves that connect to your groin, hips, and legs. This can make it hard to walk, and you may have to rest often or even limp.
- Painful sex. Many women with endometriosis (including my lovely wife) feel pain while having sex or for up to 2 days later. For some, it feels stabbing or sharp. Others describe it as an ache in the pelvic area.
- Problems with digestion including nausea, reflux, diarrhoea, and constipation
- Painful bowel movements. This one depends on the areas affected by my deep infiltrating endometriosis; it might hurt to go to the bathroom. If it’s severe, it might also cause bleeding.
Just a note, these are also all symptoms of a condition called adenomyosis which is closely linked with endometriosis in that endometriotic lesions grow within the muscle wall of the uterus. Some women are diagnosed with either endometriosis or adenomyosis or both.
3. Current theories on the cause.
The cause of endometriosis is not known. It does not happen because of anything you have done or not done.
However, genetics, the environment, and anatomical causes may contribute to the development of deep infiltrating endometriosis. Current theories on why it happens are as follows:
Retrograde menstruation – This is when some of the womb linings flow backwards and out through the fallopian tubes when a woman is having her period. The tissue then implants itself on organs in the pelvis and grows.
However, it has been suggested that most women experience some form of retrograde menstruation, so it does not explain why some women would then develop deep infiltrating endo and some do not.
This theory also doesn’t explain why endometriosis has been found in women who have had a hysterectomy and why on rare occasions it has been discovered in some men who have been exposed to oestrogen through drug treatments.
Genetic predisposition – Some research suggests that endometriosis can be passed down through the genes of family members.
Lymphatic or circulatory spread – It is thought that endometriosis tissue particles can travel around the body through the lymphatic system or in the bloodstream. This could explain why in rare cases it has been found in areas such as the eyes and brain.
Immune dysfunction – There is a theory that, for some women, their immune system is not able to fight off deep endometriosis. Many women with endometriosis appear to have reduced immunity to other conditions, but it is not known whether this contributes to deep infiltrating endometriosis or whether this is a result of endometriosis.
Environmental Causes – There has been some research to suggest that certain toxins in our environment, such as dioxin, can affect the body, the immune system, and the reproductive system, and cause endometriosis.
Studies have shown that when animals were exposed to high levels of dioxin, they developed endometriosis, but this theory has not been proven for humans.
Metaplasia – Metaplasia happens when one type of cell changes or morphs into a different kind of cell. This process usually occurs in response to inflammation and enables cells to change their surrounding circumstances to better adapt to their environment.
In the case of Endometriosis, metaplasia could explain how endometriosis cells appear spontaneously throughout the body and how they can appear in areas such as the lungs and skin.
This could also explain the appearance of endometriosis cells in women with no womb, or in men who have taken hormone treatments. During a child’s development in the womb, the process of metaplasia allows for the natural development of the human body.
Some researchers believe that this change from one type of cell to an endometriosis cell may happen as a developing baby in the womb when the baby’s womb is first forming.
Other researchers believe that some adult cells retain the ability they had as an embryo to transform into endometriosis cells.
Oestrogen Dominance – This is a recent one I have come across, there is a suggestion that endometriosis is oestrogen driven, so may be caused by women having a hormone imbalance that causes oestrogen dominance and therefore helps spread the disease.
4. Diagnosis.
Firstly, to diagnose endometriosis and other conditions that can cause pelvic pain your doctor will ask you to describe your symptoms such as heavy bleeding and chronic pelvic pain.
The problem with medical treatment is, that the vast majority of General Practitioners and General Gynaecologists don’t have enough knowledge about this chronic condition. Physical examination doesn’t reveal endo. This causes women the misery of waiting, frustration, and pain, with no clear explanation for their symptoms.

Each time a woman visits her doctor, they will immediately notice that she is in distress. The first thing they will say is something along the lines of “Have you been anxious or stressed lately? How’s your life?”
Despite the unbearable cramping pain, they may blame it on menopausal symptoms or gastrointestinal symptoms.
There is a need for more clinical trials such as a randomized controlled trial because even pelvic mri cannot reveal endometriosis 100%.
These days almost every doctor sees anxiety and depression as an explanation for everything. They never ask themselves whether there might be a physical reason for her distress.
They most often assume that the pain and symptoms must be due to stress and offer counselling or antidepressants, oral contraceptives, or pain relievers, rather than think that there might be a possibility that your pain and symptoms are causing the stress in the first place!
Women believe in doctors because they put their trust in them. They believe that the doctor should be right and sometimes this causes them to think that they are making a fuss and it must all be in their head.
They begin to think over and over, they may try different hormone treatments such as the oral contraceptives, or the Mirena coil and they may go and have some Cognitive Behavioural Therapy for stress or even take antidepressants.
They may also be sent to see a gastroenterologist or colorectal surgeon and their digestive symptoms are put down to IBS or acid reflux, which is also caused by stress.
Some of them will experience bladder symptoms and recurrent cystitis and need to see a urologist, but again nothing will be found. These women will sometimes go around and around in circles for years before it finally clicks that they could be suffering from the symptoms of endometriosis.
By this time these women will inevitably be suffering from low self-esteem, anxiety, and depression as they are being made to suffer in silence from debilitating pelvic pain.
So how is deep infiltrating endometriosis diagnosed?
There are tests to check for physical clues of deep infiltrating endometriosis, but only a specialist endometriosis surgeon who is BSGE accredited can diagnose it for sure via laparoscopy. BSGE stands for The British Society for Gynaecological Endoscopy.
General gynaecologists do not have enough experience in identifying or removing endometriotic lesions and they often miss deep infiltrating endometriosis at laparoscopy if they do find it, they also fail to treat it correctly by using ablation techniques instead of excision.
Excision is the Gold Standard treatment for deep infiltrating endo as it removes the endometriosis lesions from the root and there is less chance of it returning, whereas ablation is like shaving the top of the lesions and leaving the roots.
The tests you may be offered before laparoscopy are as follows:
Pelvic exam. During this test, your doctor manually feels (palpates) areas in your pelvis for abnormalities, such as cysts on your reproductive organs, which in terms of the illness are called “chocolate cysts” or “endometrioma”.
Or the doctor may feel some scars behind the uterus. Often, it’s not possible to feel small areas of endometriosis unless they have caused a cyst to form. The picture below reveals how it’s done.
Ultrasound. This test uses high-frequency sound waves to create images of the inside of your body.
To capture the images, a device called a transducer is either pressed against your abdomen or inserted into your vagina, which is known as a transvaginal ultrasound. Both types of ultrasound may be done to get the best possible view of the reproductive organs.
A standard ultrasound imaging test WILL NOT NECESSARILY TELL whether you have deep infiltrating endometriosis or not, but it can identify chocolate cysts/endometrioma, which are associated with endometriosis and are a sign that there may be more lesions inside your pelvic cavity.
Magnetic resonance imaging. Now, many doctors will try and mislead you by saying that MRI has a 98% chance of revealing endometriosis. This is not true! An MRI doesn’t always show it, even if it is very severe.
An MRI (magnetic resonance imaging) is an exam that uses a magnetic field and radio waves to create detailed, 3D images of the organs and tissues within your body, but endometriosis can be hidden due to the fact, that it has different shades and colours.
An MRI (magnetic resonance imaging) may show deep infiltrating endo nodules or endometrioma cysts and it may show distortion in the anatomy due to adhesions and scarring caused by endometriosis, and in this case, it helps with surgical planning.
However, the extent of the disease does not always show on MRI. In my case only the endometrioma on my ovary showed up, but the extent of the disease did not show on the MRI, yet at laparoscopy, I had it everywhere but my bowel (stage III). This has also been the case for women with stage IV deep infiltrating endometriosis.
Last, but not least is laparoscopy. A laparoscopy done by a specialist BSGE-accredited endometriosis surgeon is the only way to accurately diagnose deep infiltrating endometriosis.
The best advice I can give you is this – please don’t worry if you have the symptoms of deep infiltrating endo, but it doesn’t show up on your scans!
I know that there is a system when it comes to the NHS and that doctors have to go through a series of tick boxes before they offer you a LAPAROSCOPY, but this is THE ONLY investigation that will 100% diagnose whether or not you have endometriosis. And that is if it is done by a specialist BSGE-accredited surgeon!
Laparoscopy allows the surgeon to view the abdomen. While you’re sleeping under general anaesthesia, he makes a tiny incision near your navel and inserts a slender laparoscope, then he’s looking for signs of endometrial tissue outside the uterus.
This kind of investigation can provide information about the location and extent, and size of the endometrial implants. Your surgeon may take a tissue sample called a biopsy for further testing.
Often, with proper surgical planning, your surgeon can fully treat endometriosis during the first laparoscopy so that you will need only one procedure instead of two or more.
If endometriosis reaches stage IV it means that it spreads onto other parts of your body, such as your bowel or bladder. In that case, further surgery will be needed with a colorectal surgeon and/or a urological surgeon to remove endometriosis from these areas.
There have even been rare cases of it spreading to the liver or as far as the lungs or brain. No one knows for sure how this can happen, but there are lots of theories.
FREE Chapter of “Endo-Tool”!
an Endometriosis for Men book

5. Treatment options.
For some women medical treatment in the form of pain management and hormonal therapy helps to decrease their symptoms, but these treatments do not necessarily stop the disease from growing, although there is a theory that hormone therapy can slow the disease down.
However, hormonal therapy come with a lot of side effects and so do painkillers, and as mentioned before there is no cure. You can possibly manage its growth with hormones and give symptom relief with painkillers, but you can’t reverse it.
Getting rid of it completely involves having excision surgery, but even with excision surgery, there is a chance of it growing back. The approach which you and your doctor choose will depend on the stage, how severe your signs and symptoms are, and whether you hope to become pregnant.
Therapies used to help relieve symptoms include:
Contraceptives, such as birth control pills, patches, and vaginal rings help control the hormones responsible for the build-up of endometrial tissue each month. Using them, especially in a continuous cycle, may reduce or even eliminate pelvic pain in some cases.
Gonadotropin-releasing hormone (Gn-RH). These drugs block the production of hormones, which stimulate the ovaries. They help to lower oestrogen levels and prevent menstruation. This causes endometrial tissue to shrink.
Because they create artificial menopause, taking a low dose of oestrogen or progestin in the form of HRT along with Gn-RH may decrease menopausal side effects. Menstrual periods and the ability to get pregnant return when you stop taking these meds.
Progesterone. A variety of progesterone therapies include inserting a Mirena coil, contraceptive implants such as Nexplanon, a contraceptive injection called Depo-Provera, or a progestin pill. It can halt menstrual periods and slow the growth of endometriosis, which may relieve the signs and symptoms.
Lastly, aromatase inhibitors. They are a class of those medicines that reduce the amount of oestrogen in your body. Your doctor may recommend an aromatase inhibitor along with a progestin or a combination of contraceptives to help improve the symptoms of endometriosis.
Excision of endometriosis via laparoscopic surgery.
Excision of endometriosis and total abdominal hysterectomy – this is the last resort option and usually when there is evidence of adenomyosis (endometriosis in the muscle wall of the womb) as well as endometriosis.
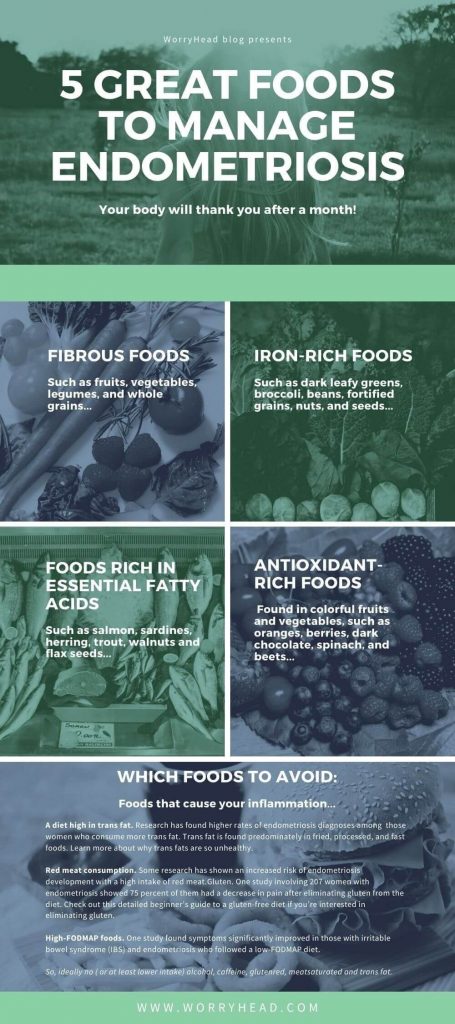
6. Nutrition and Alternative Therapies.
Nutrition
As endometriosis is an inflammatory disease, endometriosis patients should consider decreasing or eliminating inflammatory food and drinks such as the following:
- White sugar
- Dairy products
- Wheat
- Common cooking oils, trans fats, and deep-fried foods
- Processed foods
- Red meat
- Alcohol
- Caffeine
This is because artificial food additives or any foods that can cause an allergic reaction, including gluten-containing foods can cause problems for people with endometriosis. So can coffee or tobacco products. Also, non-organic, non-grass-fed meats can be a problem because of the added growth hormones they contain.

Some of the anti-inflammatory foods that should be included in your diet if you suffer from endometriosis are as follows:
- Oily fish; Salmon, Trout, Mackerel, Tuna, Sardines
- Organic meats and Eggs
- Blueberries
- Pineapple
- Papaya
- Broccoli
- Cauliflower
- Sweet potatoes
- Shiitake Mushrooms
- Legumes/Beans
- Nuts; Pistachios, Walnuts, Almonds, and Chestnuts
- Extra virgin olive oil
- Coconut oil
- Almond milk (Unsweetened) – alternative to dairy
- Cumin
- Tumeric
What you eat or don’t eat is not necessarily going to cure your endometriosis, but it’s often more effective than standard medical treatment doctors offeer because good nutrition could have a positive effect by reducing the pelvic pain you feel reducing inflammation and helping balance your hormones.
Warning! – skip the Beans and Cauliflower and go steady with the Broccoli if you suffer from IBS symptoms, and skip the Pineapple and Papaya if you suffer from Acid Reflux. I say this because women with endometriosis tend to suffer from IBS or Acid Reflux symptoms and you don’t want to make them worse!
We are all different, but these foods tend to affect me!
Alternative Therapies
Some of the alternative therapies to help manage the chronic pelvic pain, back and leg pain that some endometriosis suffers experience are as follows:
- Women’s physiotherapy
- Osteopathy
- Acupuncture
- Pilates
- Yoga
- Mindfulness and Meditation
- Cognitive Behaviour Therapy for Chronic Pain
All these therapies can help to reduce muscle pain and tension and decrease stress levels. I should mention that stress can cause endometriosis symptoms to get worse and there is also a question as to whether it may even have a role in helping the disease activate or spread in the first place since stress alone can cause hormone imbalances.
7. Fertility.
Some women with deep infiltrating endometriosis don’t have problems getting pregnant and actually experience fewer or no symptoms of the disease whilst they are pregnant since they are not having a monthly cycle to irritate the endometriosis.
However, depending on the extent of the endometriosis, particularly if it is on the ovaries, this can lead you to have trouble conceiving. If you have endometriosis and are trying for a baby, surgery may increase your chances of getting pregnant.
But if you’re still having difficulty getting pregnant, your doctor may recommend fertility treatment supervised by a fertility specialist. Such treatment ranges from stimulating your ovaries to make more eggs to in vitro fertilization.

In vitro fertilization is a process where an egg is combined with sperm outside the body to convince, in vitro. The process involves monitoring and stimulating a woman’s ovulatory process, removing an ovum or ova from the ovaries, and letting sperm fertilize them in a liquid in a laboratory condition.
Finding a doctor with whom you feel comfortable is crucial in managing and treating endometriosis. You may want to get a second opinion before starting any treatment, to be sure you know all your options and the possible outcomes. And you have every right to do so!
8. Support Groups.
One thing that I have found extremely helpful is attending a support group for women suffering from endometriosis.
This has been most vital over the last 6 months in helping me keep my mental health in check and also helped educate me on all possible options there are for treating the disease and hopefully increasing my quality of life.
The one I have been attending, along with my husband, is Endometriosis UK and both he and I can highly recommend attending their group sessions for education, support, and news on new research or treatment options. Please check out their website on the endometriosis UK website.
They not only have lots of information on their website, but they also run regular monthly support meetings at hospitals around the UK and sometimes have clinical nurse specialists and endometriosis consultants attending their meetings to do talks about endometriosis and take questions.
The sessions are free to attend, and you can attend with your partner, family member, or friend if they wish to attend with you for extra support.
There are also many other endometriosis support groups that you may find online or on social media, but Endometriosis UK is the main charity and the one which we would recommend.
Endometriosis Research
I and my hubby recently attended an Endometriosis UK information event and one of their speakers was Dr Matthew Rosser.
He has over 15 years of experience researching endometriosis, endometrial cancer, overall pelvic pain, and fibroids, and is now running a blog to help educate and inform people who wish to learn more about science and research into endometriosis. We have found his blog very interesting…
Please click on the link below to have a look at it and subscribe to updates!
www.endoupdate.co.uk
9. How endometriosis affects couples.
Hi there, it’s Lucjan again, my wife has asked me to write this part of the article to get my perspective on this subject.
But before we continue, I’d like to take a moment to strongly recommend two books, which helped my wife and her friend (fellow deep infiltrating endo sufferer) greatly with their recovery, pelvic pain, and other symptoms.
You may access these books by clicking on the book covers below…
This book has really changed my wife’s life! She struggled with her diagnosis and had nowhere to turn for knowledge and advice. This book has everything you need to know to prepare you for what’s ahead in terms of symptoms, treatment, and managing your endometriosis. We truly cannot recommend it enough! This book is definitely worth every single penny!
I listed this book because M also suffered from anxiety at that time, it helped her mindset and depression. An obsessing, ruminating, and dwelling on things may or may not happen, but this book makes it simple to understand, how to manage your fear. Your brain is a very powerful tool, and the more you work to change your mindset, the better you’re going to feel.
Out of the 100 million American women, roughly 60 percent take it for non-contraceptive reasons like painful periods, endometriosis, PCOS, and acne. While the birth control pill is widely prescribed as a quick-fix solution to a variety of women’s health conditions, taking it can also result in other more serious and dangerous health consequences.
Now, let’s continue…
As can be expected, endometriosis can have a negative impact on couples and their quality of life in complex ways. It can affect not just women with the condition, but those who are close to them, their partners, family, and friends. This chronic illness tried to impact our marriage, but we refused to let it beat us!
It is possible to have a happy and fulfilling relationship despite having endometriosis. We have a loving and very understanding, caring marriage. If you’re with someone who has a good nature, you both will be just fine. We speak here from experience!
So, what impact can endometriosis have?
Apart from the usual bleeding and pelvic pain, it can have a big impact on day-to-day life including work, parenting, simple tasks, and even your social life. This may create an extra strain on couples, and cause a lot of anxiety.
There may be an impact on her work causing financial strain as well. When it comes to social life, the feeling of being restricted can affect both partners and cause the feeling of a sense of loss.
Couples may find that seeking treatment is an ongoing battle and that itself can cause frustration for both. They might need to discuss if and how the woman would like her partner to help her make treatment decisions or not. They may also need to discuss what the partner’s role will be in consultations if they attend.
That was the case for us – my wife asked me to attend with her for support and to help her remember all the questions we needed to ask.
Sometimes it is difficult to remember everything you need to say in consultation when you have limited time and are feeling very unwell. Having your partner there to support you and prompt questions can be very helpful.
In fact, it almost seems like when my wife went on her own to consultations, she asked questions, but no one was listening, whereas when I attended with her and spoke up they seemed to take things more seriously and move things along!
However, sometimes women and their partners may have different views on how deep endometriosis should be treated and managed.
For example, research suggests, that men may be more likely to see endometriosis as something that needs to be cured, while women are likely to see it as something that can be managed long-term. Different views give different opinions and that can cause arguments.
We wouldn’t be serious here without mentioning something, that is very basic for any couple. Sex plays a very important part in any relationship.
Pelvic pain during or after sex is a common symptom of deeply infiltrating endometriosis so if you, as a woman, experience it along with some of the other symptoms, you should go and check this with your doctor as soon as possible.
Don’t forget to mention to them that what you are experiencing are symptoms of endometriosis and discuss with them the possibility of investigating your symptoms further. This can be very distressing for couples and can result in a loss of intimacy. You must remember however that sex is something that you can experience in many different forms.
It is not always about penetration guys!
Sex is about exploring what makes you both happy and you can give pleasure in many ways. If you love each other, you will find the way.
There is no man in the whole world who doesn’t like oral sex. Let’s face it, a guy will give you anything you want to receive. If he is lucky enough to have a loving partner who adores oral, there will be no issues.
When it comes to the ladies, it’s never about the orgasms (which by the way can sometimes be painful with this illness) but it is about the intimacy and the touch.
This is my personal belief but I’m happy to be challenged on that matter. I feel that men just think about the ending. Women enjoy the whole process. I think that women have a better understanding of sex, therefore they experience more pleasure.
Women get in tune with their bodies on a far deeper level than men. They don’t rush but enjoy every touch, every little sense and this slow build-up leads to higher levels of pleasure.
However, pelvic pain is not the only factor that can affect sex life. Intimacy might be affected by a range of other things, including:
- Bleeding during or after sex; general fatigue and feeling unwell
- Reduced sexual desire because of medication
- Low mood
- The stress of trying to get pregnant
- Loss of body confidence and desire
Both of you may experience feelings of guilt and sadness as well as feelings of loss associated with a lack of intimacy or closeness and affection. You may also feel hesitant and even tentative and may be reluctant to approach your partner for fear of causing pain but (as they say) there is a simple solution to this madness, it’s communication, so talk it out.
Women may face a difficult choice between avoiding sex or enduring painful sex in order to experience intimacy with their partners. My wife talked to me about it, if you talk, you will resolve every issue.
Our marriage is based on trust and open conversation. We can move mountains! So, before both of you get moody and begin thinking about it too much, just talk.
When it comes to the male partners of women who suffer from endometriosis, there is little support and information for them. Partners are often marginalized, and it is unusual for them to be asked how living alongside someone with this condition impacts them.
This is why I decided to write a book to open the conversation, and to show the perspective of those who support their partners in their struggles with endometriosis and severe pelvic pain, so remember to check “Endo-Tool” today!

Summary.
For men, research suggests that they need to be strong, and try to remain calm and in control. Men always try to hide their emotions. I tried it too. It’s in our nature, our genes, and our psyche.
Long term, however, it can be unhealthy, these experiences can reinforce ideas about masculinity, although for me it comes naturally, I’m an optimist, very confident but caring.
But I have feelings too. Endometriosis may cause feelings of frustration; some partners take on an assertive role in trying to advance the treatment.
But despite all the difficulties, deep infiltrating endo can make relationships stronger (as it did in our case), as partners may need to communicate and work together to address the impact it can have. These experiences can help them both to better understand one another, and get closer. Providing care and support can help you both appreciate one another more.
Dealing with the challenges and trying to find a way through the difficulties together can bring you closer and strengthen your relationships. We hope you will find this article helpful and use the information provided to your advantage. Don’t doubt what you feel. Your body is trying to tell you how it feels.
But let’s look closer at the point of view of a person who supports someone with endometriosis. As the husband of that special someone, I experienced various emotions, and my actions shaped my wife’s battle with endometriosis.
So I decided, I write a book to give you it all on the plate, everything you need to know from the supporter’s point of view. It will allow you, as the one who sufferer, to find out what the supporter feels and at the same time reveal to those loved ones who care for people with endometriosis, what to expect on the road ahead of you.
In the meantime, we hope you found it helpful. And if you did, please help us by sharing this article. Let’s spread the message! Thank you!


About Us
We’re just a couple of normal people. Our lives were turned upside down after an unfortunate chain of events. Get to know our story, and why I become my wife’s advocate and started my blog.