How do you know if you have endometriosis?
How do you know it?
In order to answer how you know if you have endometriosis, I split this article into 10 sections that answer the following questions:
- What is endometriosis?
- What is endometriosis commonly mistaken for?
- When do endometriosis symptoms start?
- What are the first signs of endometriosis?
- How to classify endometriosis?
- What are the 4 stages of endometriosis?
- What are the types of endometriosis?
- What are the symptoms of endometriosis?
- How can I get diagnosed with endometriosis?
- Do endometriosis type and stage affect its treatment?
My wife asked these questions when she found the worrying symptoms she’s been experiencing.
Not being sure, she rushed to the doctor, but he couldn’t confirm this disorder straight away, however, she had to make more appointments with different doctors in order to be diagnosed.
So, how do you know if you have endometriosis if even a general practitioner cannot tell you? It can be really frustrating and exhausting.
Sadly, this situation is very common amongst women who experience chronic pelvic pain, and/or heavy, painful periods.
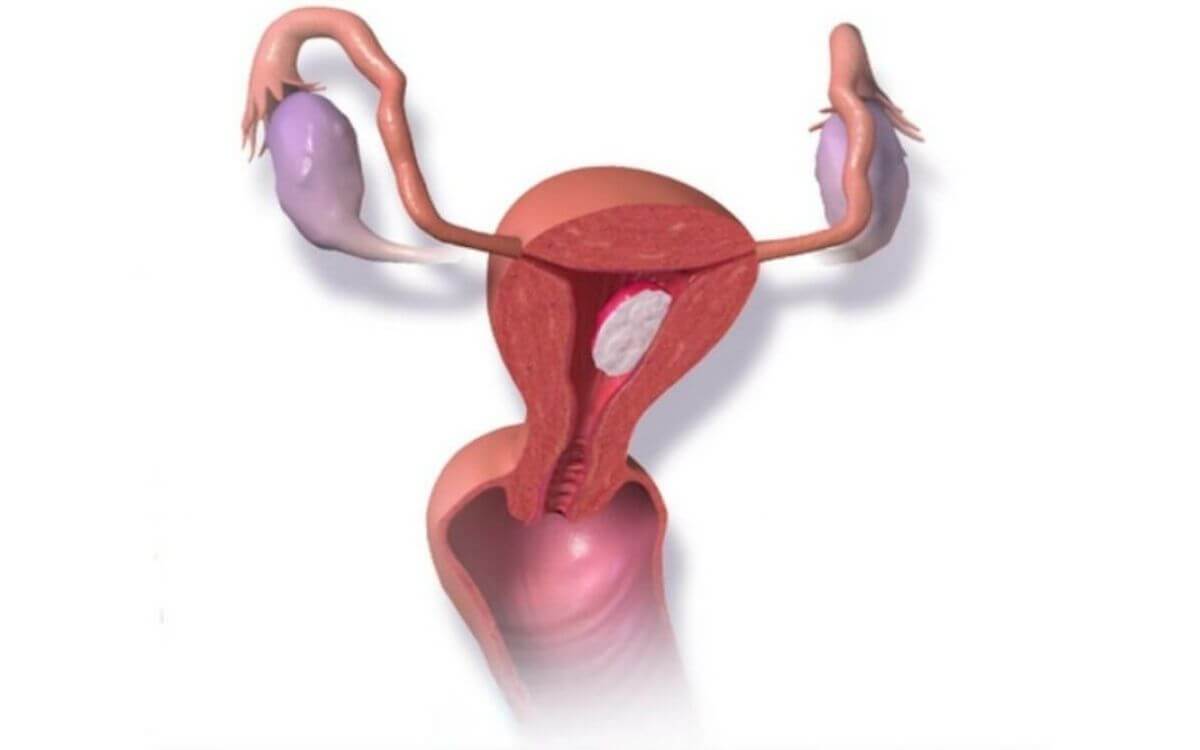
What is endometriosis?
In order to learn how do you know if you have endometriosis, we need to explain what is endometriosis?
Endometriosis is a chronic condition in which tissue similar to the lining of the womb starts to grow in other places, such as the ovaries and fallopian tubes. It is, however, a whole-body disease. Endometriosis is a long-term condition that often significantly impacts many aspects of women’s lives.
The tissue acts like endometrium tissue, which normally builds up, breaks down the bleeds monthly due to the body’s hormonal changes. But as the tissue is outside of your womb, the blood cannot exit the body as it normally would during a period.
This can cause irritation and inflammation, which leads to forming scar tissue that often causes pain.
What is endometriosis commonly mistaken for?
In order to answer how do you know if you have endometriosis it’s important to answer what is endometriosis commonly mistaken for?
There are eight such conditions, they include:
- Bladder Infection
- Pelvic Inflammatory
- Disease (PID)
- Irritable Bowel Syndrome (IBS)
- Sciatica
- Uterine Fibroids
- Polycystic Ovary Syndrome (PCOS)
- Interstitial Cystitis (IC)
- Pelvic Floor Dysfunction
In some cases, endometriosis can also be mistaken for fibromyalgia.
When do endometriosis symptoms start?
The symptoms of endometriosis can begin at any age, including early adolescence, or later in adulthood. Endometriosis symptoms may be cyclical, meaning, that symptoms come and go around the same time each menstrual cycle. They often occur around the same time as menstruation. Every woman experiences it differently.
Endometriosis symptoms may start around the same time as the first period, leading a woman to get used to the pain and think that a high level of pain is “normal” for her.
Endometriosis can be a difficult condition to diagnose early, because many people don’t have symptoms, and because confirming a diagnosis requires a surgical procedure.
My wife was on antidepressants for 18 years, she was also on the pill. All of them covered her symptoms up. She only learned about the symptoms and pain when came off them.

What are the first signs of endometriosis?
The main symptom of endometriosis is pelvic pain, which is often associated with menstrual periods. Many women experience cramping during their menstrual cycle, but those with endometriosis describe menstrual pain that’s much worse than usual. Pain also may increase over time.
Common signs and symptoms of endometriosis include:
- Painful periods (dysmenorrhea).
- Pelvic pain and cramping.
- Lower back and abdominal pain.
- Pain with and after intercourse.
- Pain with bowel movements or urination.
- Excessive, heavy bleeding.
- In some cases, it causes infertility.
- Fatigue, diarrhea, constipation, bloating.
The severity of pain is not a reliable indicator of the extent of endometriosis. Women can have mild endometriosis with severe pain, or have advanced endometriosis with little to no pain at all.
How to classify endometriosis?
There is a system of classification or staging of endometriosis. This is useful to better describe the disease, which helps develop better diagnoses and treatments.
Because endometriosis can appear in many different forms, varieties, and the extension of organs affected, a unified consensus classification system for the stages of the disease is not a simple task. The most used and best-known system is the American Society for Reproductive Medicine (ASRM).
The ASRM classification system divides endometriosis into four stages (or four grades) based on the number of lesions and depth of infiltration.
Endometriosis is classified into four stages (I-minimal, II-mild, III-moderate, and IV-severe).
Endometriosis classification depends on the location, extent, and depth of implants. Additionally, it’s classified by presence, severity, and size of adhesions and ovarian endometriomas.
What are the stages of endometriosis?
The ASRM classification uses a point system to try to quantify endometriosis lesions. This point system allows them to numerically scale the disease.
A score of 15 or less indicates minimal or mild endometriosis. A score of 16 or higher indicates moderate or severe endometriosis. However, the score (severity) of endometriosis does not always correlate with the level of pain that you experience.
This is why experts group endometriosis by stage and type. It is based on many different things, including the location, depth, size, and even the amount of tissue is present. What kind of endometriosis you have will play a big role in the future, including what kind of symptoms and treatment you will have.
There are different ways to measure this chronic disorder. Doctors usually assign points according to how much the endometrial tissue spreads. They take into account its depth and the areas of your body that are affected.
Based on the above results, endometriosis is ranked in one of four stages:
Stage 1 – minimal – where there are a few small wounds or lesions, which may be found on your organs, the tissue lining your pelvis or even your abdomen, but there’s little to no scar tissue.
Stage 2 – mild – where there are more implants than in the first stage. Additionally. they are deeper and may create some scar tissue.
Stage 3 – moderate – this stage has many deep implants. You may additionally have small cysts on either – one or two ovaries, and even thick scars called “adhesions”.
Stage 4 – severe – as the name suggests, is the most severe stage which is widespread. You have many deep and thick adhesions and there will also be large cysts on one or both ovaries.

What are the types of endometriosis?
How do you know if you have endometriosis if even experts don’t know why some people have more severe cases than others?
Endometriosis doesn’t always go from one stage to the next. If left untreated, it can remain the same over time. Or it may get worse or better. This is why, aside from stages, endometriosis is grouped by what area of the pelvis (or abdomen) it affects.
There are also four main types:
Superficial peritoneal endometriosis is the first type, in which a thin membrane, called “peritoneum”, lines your abdomen and pelvis, and covers most of your organs in these cavities. In this type, the endometrial tissue attaches to the peritoneum, which is the least severe form of endometriosis.
Endometriomas. These are dark color cysts, fluid-filled, also called “chocolate cysts” because of the way they look. They vary in size and may appear in different parts of your pelvis or/and abdomen. However, they are most common in the ovaries.
Deep infiltrating endometriosis (DIE). The endometrial tissue in this type invades your organs, either, within or outside your pelvic cavity. This may include your ovaries, rectum, bladder, and even your bowel. It’s rare, but sometimes a lot of scar tissue can bind organs together in such a way, that they become stuck in place.
This condition is called “the frozen pelvis”, and only happens to 1%-5% of people with endometriosis. Unfortunately, my wife belongs to the 1 percent, having stage IV deep infiltrating endometriosis.
Abdominal wall endometriosis. In some cases, endometrial tissue can grow on the abdominal wall. The cells may attach to a surgical incision, like one from a C-section, as it states in this source.
What are the symptoms of endometriosis?
The most common symptom of endometriosis is pain.
Because endometriosis has different types and stages, the severity of your pain may vary. Additionally, the severity of endometriosis doesn’t correlate with the severity of pain.
Sometimes, women with severe endometriosis don’t experience much pain, and women with mild type pain are extreme.
You may experience severe menstrual pain (dysmenorrhea), pain during sexual intercourse (dyspareunia), non-cyclical pelvic or abdominal pain, typically around your ovulation or on the days preceding your periods.
Lastly, there is other pain, if endometriosis spreads to other organs, which can cause pain with bowel motions or during urination, but there is also lower back and leg pain, and in rare cases of endometriosis, pain can reach your diaphragm or lungs.
Aside from pain, you may experience bleeding symptoms and changes to your bleeding pattern. The most common are heavy periods and inter-menstrual bleeding. In very rare cases of endometriosis, women can experience bleeding from the anus or in the urine.
Endometriosis infertility is not so much a symptom, but more of a clinical presentation, however, infertility is very important. Up to 70% of women who have endometriosis pain are not able to fall pregnant.
Other symptoms may be generalized and non-specific, but they still belong to endometriosis. They may include fatigue, nausea, diarrhea, constipation, migraines, and bloating (very common with endometriosis), which is often misled by IBS.
All of these feelings are pretty common and can be caused by several other conditions, however, even though they are usually the cause in 10% of women, endometriosis is not usually thought to be the cause when these symptoms are present on their own, in the absence of more specific endometriosis symptoms like cysts, discharge, bleeding, and pain.
How can I get diagnosed with endometriosis?
How do you know if you have endometriosis – by diagnosing it. But it can be difficult…
Because women experience the common symptoms of endometriosis, a large proportion of them has atypical or no symptoms at all, making it difficult for doctors to suspect endometriosis, which delays its diagnosis.
The diagnosis often takes 7 to 10 years. There’s a combination of factors that delay the diagnosis. A lack of awareness about endometriosis by doctors is the most common.
Secondly, there is a “normalization” of period pain, as if it was “a part of being a woman”. Lastly, a lack of easy and precise methods of diagnosis.
Early detection of endometriosis is important as it has the potential to reduce long-term impact on women’s and their partner’s life, improving its quality, better management, and prevention infertility.
So, how do you know if you have endometriosis?
The only way to truly diagnose endometriosis is by a surgery called “laparoscopy”.
Unfortunately, by the time doctors diagnose your endometriosis, it is often a late stage of it. Remember, that it takes many years to diagnose it because of different factors.
When you finally get your surgery, you will get general anesthesia and will be asleep. A surgeon will make a small cut and insert a small, thin viewing tool through your stomach to look for signs of endometriosis.
They often take a small sample of your tissue called “biopsy” for testing, to help rule out other causes. If the doctor discovers endometriosis lesions, he will usually cut them out.
Your doctor can only see endometriosis by laparoscopy, but again, before they order your surgery, various doctors will do other tests to rule out other conditions.
They’ll do a pelvic exam to feel for a cyst, and they may order an ultrasound or MRI to look for an endometrioma, but as it was in my wife’s case, it will probably show nothing.

Do endometriosis type and stage affect its treatment?
Presently, there is no cure for endometriosis, as the only way to cure it completely would be the complete removal of the disease.
Doctors usually decide on your treatment based on your symptoms and whether you want to get pregnant or not.
In most cases, you will start with pain medication or hormone therapy such as birth control pills. Doctors used to think hormone therapy didn’t work for deeply infiltrating endometriosis, but recent research suggests that they do.
If these treatments don’t help (which they don’t because they just mask the symptoms), you may need surgery to remove the endometrial implants. This can be done by laparoscope or by abdominal surgery.
Another option for women who don’t want to get pregnant is to surgically remove the uterus.
This is called a hysterectomy, leaving your ovaries intact. However, it could be paired with an oophorectomy, where the surgeon takes out your ovaries too.
Treatments for endometriosis, including the surgery, have the potential to reduce the symptoms associated with it, but there is a possibility that over time endometriosis will grow back and related symptoms may return.
The objective of laparoscopic surgery is to remove the areas that contain endometrial tissue, these areas are excised using special instruments. If the ovaries contain endometriotic cysts, these are also excised or ablated.
Ongoing hormonal treatment is often used after your surgery (but not necessary) to enhance the reduction of symptoms, and reduce the risk of endometriosis recurrence in the future. Lastly, some women may require both surgery and then IVF.
The decision to operate is based on your circumstances, but also the presence or absence of pain and the availability of other treatment options.
Every woman is unique and decides what to do depending on her age, severity of symptoms, and desire for fertility.
Summarizing how do you know if you have endometriosis…
That’s it for how do you know if you have endometriosis. I hope you found it helpful.
Endometriosis is a disorder with a very late diagnosis rate. It cannot be cured and is highly disabling not only for the women who suffer from endometriosis but also for those who support them.
The costs associated with its treatment are significant, affecting you as a couple, your family, your finances, and your social life. The delay in the diagnosis of endometriosis has consequences on the quality of your life, including social, personal, and working life.
Furthermore, like in my wife’s case, the fear that this situation could affect life with your partner and the uncertainty about the possibility of having children, are two of the most frequent reasons why men leave their women.
This has psychological repercussions and if this happened to you, it is advisable that you reach for psychological support.
Until then, understanding how endometriosis affects your life can help you create a plan to cope with this disease. To help you with that, I wrote an “Endo-Tool, Endometriosis for Men” e-Book! I give you the 1st chapter FREE. It contains 20 pages filled with value, such as:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
Get FREE “Endo-Tool”
Endometriosis for Men e-Book



About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…