Checklist for fibromyalgia symptoms. (Updated 3rd Nov 2023)
As a husband of a chronically ill wife who suffers from endometriosis and fibromyalgia, and also as a blogger, I understand the importance of providing accurate and useful information to help individuals cope with chronic conditions like fibromyalgia. In this article, I will be sharing a comprehensive checklist for fibromyalgia symptoms.
I updated this article from the 18th of November 2020 to the 3rd of November 2023, as it was long overdue. Now, let me begin with some basic facts and then I delve deeper into the topic...
A checklist for fibromyalgia symptoms includes widespread pain, fatigue, sleep disturbances, cognitive difficulties, numbness or tingling, and often co-occurring conditions like IBS, headaches, and depression. Diagnosis may require a doctor’s evaluation of these symptoms.
With the checklist provided in this article, people, particularly male partners, can have a better understanding of the common symptoms associated with fibromyalgia and empower themselves to support their female partners who are living with this condition.
Stay tuned for this informative and helpful guide on fibromyalgia symptoms checklist.
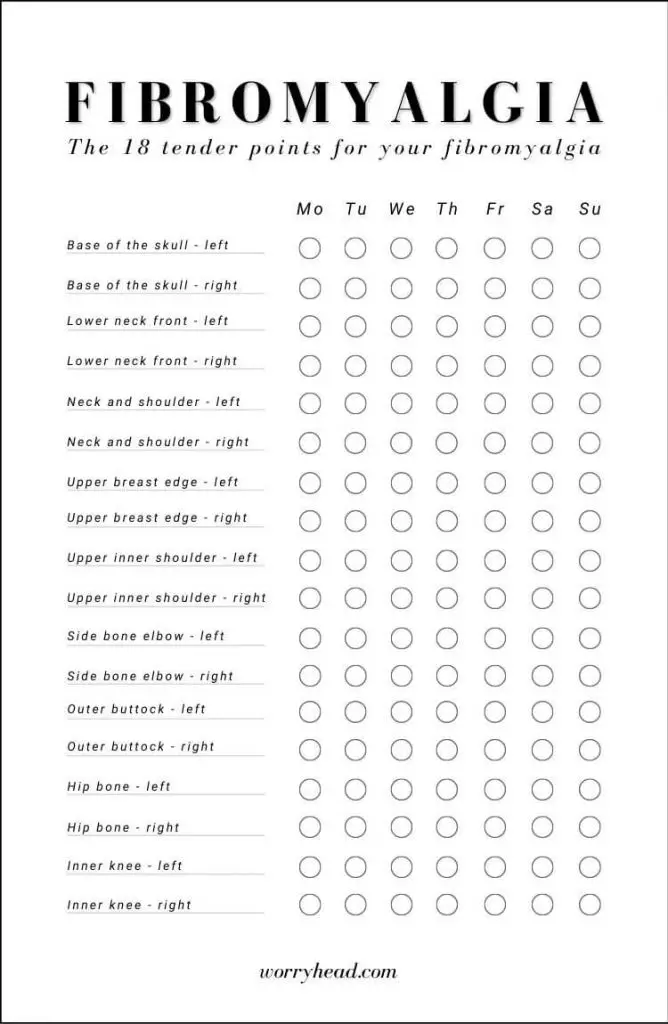
It’s worth remembering, that aside from the checklists for fibromyalgia symptoms we should also look for fibromyalgia tender points. The checklist for fibromyalgia tender points includes:
- The back of your neck.
- Your elbows.
- The front of your neck.
- Your pelvis.
- Lower back.
- Knees.
- Upper back.
- Shoulders.
- Your chest.
- FREE checklist for fibromyalgia symptoms infographic and more!
- My wife's medical conditions…
- Understanding fibromyalgia: a brief overview.
- Chronic pain: the primary symptom of fibromyalgia.
- Fatigue and sleep disturbances.
- Cognitive difficulties: "Fibro Fog"!
- Mood disorders: depression and anxiety.
- Sensory overload: heightened sensitivity.
- Digestive issues: the gut-brain connection.
- Physical limitations: reduced mobility and function.
- Headaches and migraines.
- Temperature sensitivity: hot and cold intolerance.
- Fluctuating symptoms: the nature of fibromyalgia.
- When to seek medical help?
- Supporting your partner: tips for coping and communication.
- Checklist for fibromyalgia symptoms and tender points.
- The complexity of fibromyalgia symptoms…
- Treatment of fibromyalgia symptoms…
- Conclusion on the checklist of fibromyalgia symptoms.
FREE checklist for fibromyalgia symptoms infographic and more!
I wanted to begin with two gifts, so below you will find a FREE fibromyalgia tender points infographic and a FREE diagnosis checklist of these points for you to download.

My wife’s medical conditions…
Aside from fibromyalgia, my wife, M, also suffers from stage IV endometriosis. Primarily she was diagnosed with endometriosis and fibromyalgia occurred the following year.
While my wife experienced pain on and off for many years in the past, this pain used to be located in her pelvic area, however, over time, the pain has progressed to her legs, and spine, eventually becoming widespread, more consistent, and becoming a daily struggle.
But how common is it to be struggling with multiple medical conditions?
When it comes to chronic illness, many women experience both fibromyalgia and endometriosis and have a higher risk of having other autoimmune diseases such as IBS and chronic fatigue syndrome, anxiety, or depression as well as more hospitalizations. Additionally, my wife experienced all of them, plus Obsessive-Compulsive Disorder. She also has other gastric problems like acid reflux and heartburn, and she also suffers from Iron anemia and Magnesium deficiency.
Studies prove that women who were diagnosed with endometriosis after surgery reported a high prevalence of fibromyalgia. That was the case with my wife. The trauma of endometriosis brought fibromyalgia. According to researchers from Southwest Spine and Pain Center, “women with endometriosis were twice as likely to have fibromyalgia than those who did not have the condition.
In the endometriosis community, I’ve met many women who suffer from fibromyalgia and endometriosis simultaneously.
Endometriosis is a condition where tissue similar to the lining of the womb starts to grow in other places, such as the ovaries and Fallopian tubes. This condition affects 1 in 10 women worldwide. It’s a life-long illness that can have a significant impact on your life in many ways.
If you want to learn more about it, feel free to check my “Endo-Tool”.
Understanding fibromyalgia: a brief overview.
Before diving into the checklist, it’s important for me to provide a brief overview of fibromyalgia. Fibromyalgia is a chronic condition that primarily affects the muscles and soft tissues, causing widespread pain and tenderness throughout the body. While anyone can develop fibromyalgia, it is more common among females, with a 7:1 female-to-male ratio. The condition can also present with a range of symptoms beyond pain and tenderness, which we will discuss in more detail below.
Fibromyalgia symptoms.
The symptoms of fibromyalgia can vary from person to person and may come and go over time. Common symptoms of fibromyalgia in females include:
- Chronic pain and tenderness
- Fatigue and sleep disturbances
- Cognitive difficulties, commonly referred to as “fibro fog”
- Mood disorders, such as depression and anxiety
- Sensory overload, with heightened sensitivity to various stimuli
- Physical limitations and reduced mobility
- Headaches and migraines
- Temperature sensitivity, with intolerance to both hot and cold
- Digestive issues, such as irritable bowel syndrome (IBS)
Diagnosing fibromyalgia.
Diagnosing fibromyalgia can be challenging, as there are no specific tests that can confirm the condition. Instead, healthcare professionals rely on a combination of a patient’s reported symptoms and a physical examination to diagnose fibromyalgia. It’s essential to seek medical evaluation if you are experiencing symptoms of fibromyalgia.
While there is no cure for fibromyalgia, there are treatment options available to manage and alleviate symptoms. We will discuss strategies for managing symptoms throughout this article.
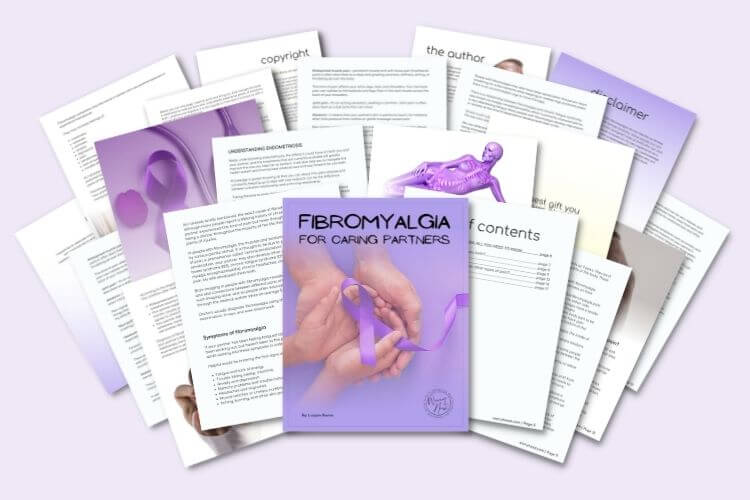
If you want to learn more about fibromyalgia, I wrote a “Fibromyalgia for Caring Partners” e-Book.
You can get the 3 First Chapters of the e-Book for FREE, and if you like it, you’ll get a Whopping 33% Discount on the Whole Book, plus discounts on other helpful tools. You have nothing to lose but a lot to gain.
These chapters alone explain how to accept the new normal, and understand fibromyalgia, and its diagnosis. They include:
- The new you.
- The new her.
- The new reality.
- Introduction to fibromyalgia.
- What is fibromyalgia?
- The early days.
- When you first realize something is wrong.
- Spotting the signs that something is wrong.
- Coming to terms with a chronic illness.
- The role of partner in fibromyalgia.
- The process of getting diagnosed.
Get Your 3 FREE Chapters!
Fibromyalgia for Caring Men
Fibromyalgia symptoms in females.
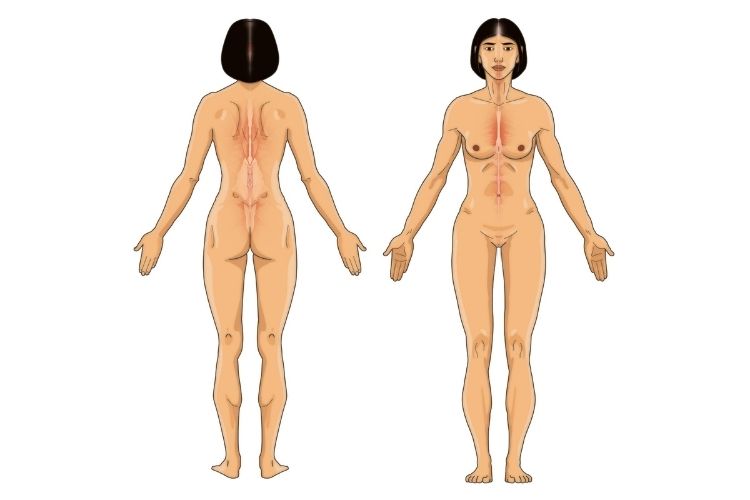
What differentiates fibromyalgia symptoms in females from symptoms in men is the presence of “tender points” which can be localized in the neck, chest, elbows, or other parts of the body. They can become more painful when pressure is applied to them.
Other particular symptoms in women include migraines, abdominal pain, pelvic pain, breast tenderness, and difficulty sleeping. Women are also more prone to depression and anxiety, but not only that, unlike men, women may have more cognitive issues such as difficulty concentrating and memory problems.
Like in the case of my wife, many women also suffer from endometriosis alongside fibromyalgia, which makes the symptoms overlap, making it more difficult to diagnose.
Women who suffer from fibromyalgia experience fatigue and difficulty concentrating, which can lead to problems performing daily tasks. Since fibromyalgia is a chronic illness, symptoms can come and go over time, so it’s important to be aware of them.
Finally, I want to remind you that fibromyalgia is a complex condition and it’s important to talk to your doctor about any symptoms that you experience.
Chronic pain: the primary symptom of fibromyalgia.
As mentioned earlier, chronic pain is the primary symptom of fibromyalgia and can manifest in different ways. It can be described as a deep, dull ache, a burning sensation, or a shooting pain. Some individuals may experience pain in specific areas, while others may feel pain all over their body.
It is essential to understand the different types of pain that fibromyalgia can cause, as this can help in effectively managing the condition. Here are some common types of pain associated with fibromyalgia:
| Type of pain | Description |
|---|---|
| Tender points | The presence of tender points on certain areas of the body, which hurt when pressure is applied. |
| All-over pain | Pain felt throughout the entire body, often described as a deep ache or a burning sensation. |
| Headaches | Recurrent headaches or migraines that can be intense and sometimes debilitating. |
| Muscle pain | Pain, stiffness, and soreness in the muscles, especially after physical activity or extended periods of inactivity. |
In addition to these types of pain, fibromyalgia can also cause pain in specific locations, such as the neck, shoulders, back, hips, and legs. However, it’s important to note that pain may vary from person to person, and some individuals may experience additional types or locations of pain.
If you or a loved one are experiencing chronic pain and other symptoms of fibromyalgia, it’s crucial to seek medical attention. A healthcare professional can evaluate your symptoms and provide an accurate diagnosis and treatment plan.
FREE chronic pain body map.
When diagnosing, doctors may not immediately consider fibromyalgia when evaluating these types of symptoms, because pain is also common with many other conditions, like endo or CFS.
That’s one reason why it takes an average of five years for people with fibromyalgia to get diagnosed and seven to eight years on average, to get diagnosed with endometriosis.
Knowing the type and location of pain you have, may help your doctor diagnose you earlier. The faster you get diagnosed, the sooner you can get started on a treatment to relieve your symptoms.
But as it was in the case of my wife, it took a while for her to pinpoint exactly where, and what kind of pain she felt at any moment. My wife used to get frustrated trying to explain her pain, my lack of understanding wasn’t helpful either. After all, I’m a man, and I don’t experience what she’s going through.
I decided to create a chronic pain body map that you can also download below for FREE.
Fatigue and sleep disturbances.
Fibromyalgia can cause persistent fatigue and sleep disturbances that can significantly impact an individual’s quality of life. In fact, sleep problems are so common that they are included in the diagnostic criteria for fibromyalgia. Here are some of the ways in which fibromyalgia can affect sleep.
Frequent waking.
Individuals with fibromyalgia often experience interruptions in their sleep, leading to frequent waking throughout the night. These interruptions can be caused by pain, restless leg syndrome, or other factors, and can result in feeling fatigued and unrefreshed upon waking in the morning.
Difficulty falling asleep.
Fibromyalgia can cause difficulty falling asleep due to pain, anxiety, or other factors. This can lead to frustration and anxiety about going to bed, making it even more challenging to relax and fall asleep.
Light sleep.
Even when individuals with fibromyalgia are able to fall asleep, the quality of their sleep can be affected. They may spend more time in light sleep than in deeper, more restorative sleep, causing them to wake up feeling fatigued and unrefreshed.
Strategies for managing sleep disturbances.
Fortunately, there are strategies that can help manage sleep disturbances associated with fibromyalgia:
- Establish a consistent sleep schedule, going to bed and waking up at the same time every day.
- Create a comfortable sleep environment that is cool, dark, and quiet.
- Avoid caffeine, alcohol, and large meals close to bedtime.
- Practice relaxation techniques like deep breathing or progressive muscle relaxation before bed.
- Consider cognitive-behavioral therapy or other forms of therapy to address anxiety or other emotional factors that may be interfering with sleep.
It’s important to consult with a healthcare professional if sleep disturbances persist, as they may recommend other treatment options like medication or referral to a sleep specialist.
Cognitive difficulties: “Fibro Fog”!
One of the most challenging symptoms of fibromyalgia is the cognitive difficulties it can cause. Many individuals, including my partner, experience what is commonly referred to as “fibro fog.”
Fibro fog can manifest as difficulty concentrating, memory problems, mental fatigue, and trouble with word recall. It can be frustrating for both the person experiencing it and their loved ones, as it can make even simple tasks feel overwhelming.
If your partner is experiencing fibro fog, it’s essential to be patient and understanding. Encourage them to take breaks when they need to, and avoid pressuring them to remember things they may have forgotten.
One helpful strategy for managing cognitive symptoms is to create a routine and stick to it as much as possible. This can help reduce decision-making fatigue and provide structure to the day.
Another useful approach is to break down tasks into smaller, manageable steps. For example, if your partner needs to go grocery shopping, break down the task into a list of what needs to be purchased, which stores to visit, and what timeframe they have available to complete the task.
It’s also crucial to communicate effectively with your partner about their cognitive symptoms. Encourage them to share their experiences with you and let them know that you are there to support them. By working together, you can find strategies that work for both of you in managing the challenging cognitive symptoms of fibromyalgia.
Mood disorders: depression and anxiety.
Another common symptom of fibromyalgia is the onset or worsening of mood disorders, particularly depression and anxiety. As the partner of someone living with fibromyalgia, it’s essential to understand the effects of these mood disorders and how to support your loved one in managing them.
Fibromyalgia symptom tracker: When tracking the emotional symptoms of fibromyalgia, it’s vital to monitor the individual’s mood, energy levels, and overall sense of well-being. Tracking frequency and duration can help identify patterns or triggers that may contribute to mood changes.
Living with fibromyalgia can take a toll on one’s mental health, leading to depression and anxiety. These mood disorders can be caused by the chronic pain and discomfort associated with fibromyalgia, as well as the limitations it imposes on daily activities and social interactions. It’s crucial to remember that these mood disorders are not a sign of weakness; rather, they are a natural response to living with a chronic illness.
Fibromyalgia symptom evaluation: If you notice that your partner is experiencing persistent feelings of sadness or hopelessness, losing interest in their hobbies or activities, or having difficulty sleeping or concentrating, it may be time to consult with a healthcare professional. Depression and anxiety are treatable conditions, and seeking medical help can provide much-needed relief.
As a partner, there are various ways to support your loved one in managing their mood disorders. The first step is to listen and validate their feelings. It’s essential to provide a safe and non-judgmental space for them to share their emotions and express their concerns. Encourage them to seek professional help if necessary, and offer to accompany them to appointments.
Additionally, supporting your partner’s physical health can also positively impact their mental health. Encourage them to maintain a healthy diet, engage in regular physical activity as appropriate, and get adequate sleep. These lifestyle changes can help reduce the severity of fibromyalgia symptoms and improve overall well-being.
Finally, practicing self-care together can be a powerful way to support each other. Try taking a relaxing bath together, engaging in a hobby or activity you both enjoy, or spending quality time outdoors. Finding ways to reduce stress and promote relaxation can go a long way in managing the emotional symptoms of fibromyalgia.
If you want more in-depth information about how to support your partner with her chronic conditions and how to cope with the new normal in your relationship, I wrote a “Supporting a Chronically Ill Partner” e-Book.
You can get the 1st Chapter of the e-Book for FREE, and if you like it, you’ll get a Whopping 33% Discount on the Whole Book, plus discounts on other helpful tools. You have nothing to lose but a lot to gain!
The first chapter alone contains a lot of information for both of you about acknowledging the struggles, including:
- A word to your partner.
- A word to you.
- Stepping on eggshells.
- Understanding her needs.
- How to acknowledge having a chronically ill partner?
- Acknowledging can be hard.
- 15 tips on how to do it!
Get the 1st Chapter FREE!
Chronic Illness for Partners
Sensory overload: heightened sensitivity.
Individuals with fibromyalgia often experience heightened sensitivity to various stimuli, such as light, sound, touch, and temperature. This can be overwhelming and lead to further discomfort and fatigue. Understanding these sensory symptoms is crucial for effectively managing fibromyalgia.
Light sensitivity.
Also known as photophobia, light sensitivity is a common symptom in fibromyalgia. Bright or flickering lights can trigger headaches and migraines and worsen fatigue. If you’re experiencing light sensitivity, it may be helpful to:
- Avoid fluorescent or bright lighting
- Wear sunglasses or a hat when outside
- Use a dimmer switch or soft lighting in your home
Sound sensitivity.
Individuals with fibromyalgia may also experience sensitivity to loud or sudden noises, leading to anxiety and fatigue. If you’re experiencing sound sensitivity, it may be helpful to:
- Avoid loud places, such as concerts or busy restaurants
- Use earplugs or noise-cancelling headphones
- Ask others to speak softly or avoid sudden noises around you
Touch sensitivity.
Individuals with fibromyalgia may experience hypersensitivity to touch, making even light pressure uncomfortable. This may also lead to skin irritation and pain. If you’re experiencing touch sensitivity, it may be helpful to:
- Wear loose-fitting, soft clothing
- Avoid tight clothing or clothing with rough seams
- Use soft blankets and pillows
Temperature sensitivity.
Fibromyalgia can cause individuals to have difficulty regulating body temperature, leading to intolerance to both heat and cold. This can be uncomfortable and exacerbate other symptoms. If you’re experiencing temperature sensitivity, it may be helpful to:
- Use fans or air conditioning to cool down
- Wear light, breathable clothing during hot weather
- Use heating pads or warm blankets to warm up during cold weather
By understanding and managing sensory symptoms, individuals with fibromyalgia can reduce discomfort and improve their overall quality of life.
Digestive issues: the gut-brain connection.
As previously mentioned, digestive issues are common among individuals with fibromyalgia. This is due to the strong connection between the gut and the brain. In fact, the gut is often referred to as the “second brain” due to the vast number of neurons it contains.
Symptoms of digestive issues often include abdominal pain, bloating, constipation, and diarrhea. These symptoms can significantly impact an individual’s quality of life and make it challenging to manage other symptoms associated with fibromyalgia.
If you suspect that you are experiencing digestive issues related to fibromyalgia, keeping a symptom diary can be incredibly helpful. This will allow you to identify patterns and potential triggers for your symptoms and provide valuable information for your healthcare provider.
In addition to keeping a symptom diary, making dietary changes can also be beneficial for managing digestive symptoms. For example, reducing your intake of processed foods and sugar can help rebalance your gut microbiome and alleviate symptoms.
It is also essential to stay hydrated and maintain a healthy level of physical activity. Exercise not only helps with digestion but can also improve mood and reduce overall fibromyalgia symptoms.
Physical limitations: reduced mobility and function.
One of the most challenging aspects of fibromyalgia is the impact it can have on physical abilities. The chronic pain, fatigue, and cognitive difficulties associated with fibromyalgia can lead to reduced mobility, limited range of motion, and decreased overall function.
The physical limitations of fibromyalgia can vary from person to person and can include:
- Pain and stiffness in joints and muscles
- Difficulty with balance and coordination
- Decreased endurance and stamina
- Sensitivity to touch and pressure
These symptoms can make it difficult to perform everyday tasks such as walking, sitting, and standing. Individuals with fibromyalgia may also struggle with household chores, personal care, and employment responsibilities.
Effective management of fibromyalgia symptoms can help improve physical abilities and maintain an active lifestyle. A combination of medication, physical therapy, and lifestyle modifications can help increase mobility, reduce pain, and improve overall function.
Physical therapy.
Physical therapy is an essential component of fibromyalgia symptom management. A physical therapist can create a personalized exercise program that focuses on improving flexibility, range of motion, and strength.
Stretching exercises, low-impact aerobic activity, and strength training can help improve endurance and reduce pain and stiffness. Physical therapy can also include massage, heat therapy, and other techniques to alleviate pain and improve circulation.
Lifestyle modifications.
Lifestyle modifications can also help improve physical abilities and reduce fibromyalgia symptoms. Individuals with fibromyalgia may benefit from:
- Reducing stress and anxiety
- Getting adequate sleep and rest
- Eating a balanced and nutritious diet
- Avoiding trigger foods and substances
- Wearing supportive shoes and clothing
- Using assistive devices when necessary
By incorporating these lifestyle changes, individuals can better manage their symptoms and improve overall physical function.
Headaches and migraines.
Headaches and migraines are a common symptom experienced by individuals with fibromyalgia. These headaches can range from mild to severe and may occur frequently or infrequently. It’s essential to track headache patterns and potential triggers to better manage them.
If you are experiencing headaches with any of the following symptoms, seek medical care:
- Sudden and severe onset
- Accompanying fever, vomiting, or confusion
- Worsening headache over time
Keeping a headache diary can help identify potential causes and allow for better management of headaches and migraines. Consider including the following information:
- Date and time of headache onset
- Duration and intensity of headache
- Associated symptoms, such as nausea or sensitivity to light or sound
- Potential triggers, such as stress or certain foods
- Treatments used and their effectiveness
It’s crucial to communicate your headache patterns and symptoms to your healthcare provider to ensure effective management and treatment.
Temperature sensitivity: hot and cold intolerance.
One of the most challenging symptoms of fibromyalgia is temperature sensitivity, or the inability to regulate body temperature. Individuals with fibromyalgia may experience intolerance to both heat and cold, which can be very uncomfortable and disruptive to daily life. For me, this symptom can be particularly challenging during the winter months when the cold weather exacerbates my pain and stiffness.
When it comes to hot intolerance, many individuals with fibromyalgia experience increased sweating, dizziness, and fatigue in hot weather. It’s important to stay hydrated and dress in light, breathable clothing to stay comfortable. If possible, try to stay in air-conditioned spaces during the hottest parts of the day.
Cold intolerance, on the other hand, can cause individuals with fibromyalgia to feel chilled to the bone, even in mild weather. Layers are your best friend during this time, and it’s important to dress in warm clothing and keep yourself dry. You may also want to consider investing in a heating pad or heated blanket to help manage your symptoms.
Managing temperature sensitivity.
While temperature sensitivity can be a challenging symptom to manage, there are strategies that can help reduce its impact on your daily life.
- Keep a log of your temperature-related symptoms. This can help you identify patterns and triggers so you can take steps to avoid them in the future.
- Stay mindful of your body’s temperature needs. Pay attention to how you feel and adjust your clothing or surroundings as needed.
| Hot Intolerance | Cold Intolerance |
|---|---|
| Stay hydrated | Dress in layers |
| Avoid direct sunlight | Keep yourself dry |
| Seek out air-conditioned spaces | Invest in a heating pad or heated blanket |
By staying aware of your temperature-related symptoms and taking steps to manage them, you can minimize the impact of this challenging symptom on your daily life.
Fluctuating symptoms: the nature of fibromyalgia.
Living with fibromyalgia can be a rollercoaster of symptoms that can fluctuate in intensity and vary from day to day. It’s important to understand the nature of this condition and why it can be challenging to manage.
Fibromyalgia is typically a chronic condition that can cause a wide range of symptoms that affect the entire body. These symptoms can come and go, making it difficult to predict when they will occur and how severe they will be. Some days, individuals with fibromyalgia may feel relatively pain-free and energetic, while other days they may struggle to get out of bed due to chronic pain and fatigue. This unpredictability can make it challenging to plan daily activities or maintain a consistent routine.
Additionally, fibromyalgia symptoms can be exacerbated by various triggers, such as stress, lack of sleep, or changes in weather. These triggers can make it difficult to identify the root cause of symptoms and manage them effectively.
It’s essential to keep track of symptoms and identify patterns to develop effective coping strategies. Using a fibromyalgia diagnosis checklist or an autoimmune disease symptom checklist can be helpful in tracking symptoms and identifying patterns. This information can be shared with healthcare providers to develop a personalized treatment plan that addresses the individual’s specific needs.
Finally, it’s crucial to recognize that managing fibromyalgia symptoms is an ongoing process that requires patience, persistence, and a willingness to try different approaches. With the right support network and management strategies, individuals with fibromyalgia can lead fulfilling lives despite the challenges this condition presents.
When to seek medical help?
While fibromyalgia is a chronic condition, it’s essential to understand when to seek medical help. As a partner, it’s important to be aware of the red flags that may indicate the need for further evaluation and treatment. Below are some of the warning signs to look out for:
- Severe or unusual headaches
- New or worsening neurological symptoms, such as weakness or numbness in the limbs
- Unexplained weight loss or gain
- Changes in bowel or bladder habits
- Sharp, stabbing pain in one specific area of the body
- Fever or other signs of infection
If you or your partner experience any of these symptoms, it’s essential to consult a healthcare professional for further assessment and treatment. It’s important to keep track of any new or unusual symptoms and communicate them to your doctor.
When to visit the emergency room?
In rare cases, fibromyalgia symptoms can be severe enough to warrant a visit to the emergency room. If you or your partner experience any of the following, seek emergency medical attention immediately:
- Chest pain or difficulty breathing
- Severe abdominal pain
- Fainting or loss of consciousness
- Sudden and severe dizziness or vertigo
- Seizures or convulsions
Remember, even though fibromyalgia is a chronic condition, it’s important to stay vigilant and seek medical help when necessary. Regular communication with your healthcare provider and keeping track of symptoms can help manage the condition effectively.
Supporting your partner: tips for coping and communication.
Living with fibromyalgia can be incredibly challenging, not just for the individual experiencing the symptoms, but also for their partners. As someone who has supported a loved one with this condition, I understand the toll it can take on a relationship. However, there are ways that you can support your partner and navigate the difficulties together.
Practice empathy and understanding.
By acknowledging the impact of fibromyalgia on your partner’s life, you are showing that you care about their well-being. Don’t dismiss or downplay their symptoms, and try to understand the challenges they face every day. Empathy and understanding are key to showing support and fostering a strong relationship.
Communicate openly and honestly.
Communication is essential in any relationship, but it’s especially important when dealing with a chronic condition like fibromyalgia. Encourage your partner to express their feelings and needs openly and honestly, and be willing to do the same. This way, you can work together to find solutions and support each other through difficult times.
Be flexible and adapt to fluctuating symptoms.
Fibromyalgia symptoms can fluctuate in intensity and vary from day to day. This can be frustrating for both the individual with fibromyalgia and their partner. However, being flexible and adaptable can help you navigate these changes. For example, if your partner is experiencing a particularly bad day, be willing to adjust plans or take on more responsibilities to help them manage their symptoms.
Encourage self-care.
Self-care is crucial for managing fibromyalgia symptoms. Encourage your partner to prioritize their well-being and engage in activities that promote physical and emotional health. This could be as simple as taking a relaxing bath or going for a walk together. By supporting your partner’s self-care, you are showing that you care about their overall health and happiness.
Seek support and resources.
Support groups, online forums, and educational resources can be valuable tools for both you and your partner. These resources can provide information about fibromyalgia symptom management, tips for coping with the emotional toll of the condition, and opportunities to connect with others who are going through similar experiences. By seeking out support and resources, you can better support your partner and strengthen your relationship.
Supporting a partner with fibromyalgia can be challenging, but it’s also an opportunity to deepen your
Checklist for fibromyalgia symptoms and tender points.
I’ve given you plenty of freebies already, but I need to get to the point and expand a little bit on the checklist of fibromyalgia symptoms and the checklist of tender points that fibromyalgia is associated with.
These tender points are areas on the body where people with fibromyalgia feel more pain or soreness than usual. They are located in specific spots along the spine, neck, and shoulders.
They can also be found in other parts of the body such as hips, elbows, and knees. When touched lightly or pressed on with a finger, they are often painful to people with fibromyalgia.
For some people, these tender points may come and go over time, while for others they may be a permanent part of the fibromyalgia symptom checklist. It is important to note that these tender points are not always indicative of fibromyalgia, as they can also be caused by other conditions.
Let’s dive first into the symptoms of fibromyalgia!
The checklist for fibromyalgia symptoms.
The checklist for fibromyalgia symptoms includes:
- Fatigue: This symptom refers to feeling exhausted for no apparent reason. People with fibromyalgia often describe it as feeling like their energy has been “sucked out” of them.
- Pain: This can range from mild discomfort to severe pain in the muscles and joints. The pain often seems to radiate from one part of the body over time or move around from place to place.
- Cognitive issues: Many people with fibromyalgia experience “fibro fog”, which is a lack of mental clarity and difficulty concentrating.
- Sleep problems: People with fibromyalgia often have trouble getting enough restful sleep, which can cause daytime fatigue.
- Anxiety and depression: These symptoms are common among people with fibromyalgia. They can contribute to a feeling of overall distress or unhappiness that interferes with daily life.
The checklist for fibromyalgia tender points.
The checklist for fibromyalgia tender points includes:
- The back of your neck: People with fibromyalgia are more likely to experience tenderness in this area, which is known as the occiput. This area is located at the base of your skull and can be very painful when touched.
- Your elbows: Pain in this area is common in people with fibromyalgia and can be caused by inflammation in the muscles or joints around the elbow joint.
- The front of your neck: The sternoclavicular joint, which connects your collarbone to your breastbone, may also become tender or painful for people with fibromyalgia.
- Your pelvis: You may feel pain or stiffness in this area due to muscle tension in your hips or lower back.
- Lower back: Fibromyalgia can cause discomfort or pain in the lower back due to tightness in the muscles around it.
- Knees: Pain or tenderness in the knee joint can be caused by inflammation in the joint, due to fibromyalgia.
- Upper back: Tension and soreness in this area can be a result of neck stiffness or muscle strain from carrying too much weight.
- Shoulders: Muscle tension, inflammation, and fatigue can cause pain in your shoulders as well.
- Your chest: Fibromyalgia can cause pain in this area due to tightness in your chest muscles or joint inflammation around the ribs.
The complexity of fibromyalgia symptoms…
Fibromyalgia symptoms are complex and can vary in intensity and frequency. It is important to remember that fibromyalgia is a serious condition, and your checklist of symptoms should be taken into account when seeking treatment.
Pain and tenderness in muscles and joints throughout your body can shift from place to place, but to meet the criteria for a diagnosis, the person needs to have experienced pain for at least three months to be considered chronic.
Such pain must also be in a specific number of body parts and be above a specific severity score. Important is that you do not have other conditions such as arthritis or endometriosis, that could explain the pain.
Fibromyalgia causes a number of other symptoms, such as fatigue lack of energy trouble sleeping depression or anxiety memory problems, and fibro-fog (trouble with concentrating). Headaches, muscle twitches, cramps, numbness, tingling in the hands and feet, itching, burning, and other skin problems can be the symptoms of fibromyalgia.
Pain belongs to the most severe symptoms and can be very intense, and constant. It can be so severe that keeps you home from work and other activities. But again, it can be the same for endometriosis.
Fibromyalgia can also cause intense emotional symptoms such as anxiety and depression. Fatigue can have one of the biggest impacts on your mental health.
Chronic fatigue affects more than 90% of people with fibromyalgia. It isn’t usual tiredness. It can actually cause very serious exhaustion, draining your body of energy, and turning even the simplest activity into a chore.
Some people with fibromyalgia experience also uncomfortable symptoms of irritable bowel syndrome, commonly known as IBS. These symptoms are diarrhea with or without constipation, belly pain, belly bloating due to gas, and nausea.
Up to 70% of people notice regular tension or migraine headaches, which are often extremely severe. More unusual symptoms of fibromyalgia are symptoms that you might not expect, but they can still occur:
- excess sweating
- easy bruising
- swelling
- sensitivity to noise
- sensitivity to light
- sensitivity to temperature
- jaw pain
- chest pain
- bladder pain
- urgent need to urinate
- food allergies
- stuffed nose
- wheezing
- vomiting
How can fibromyalgia pain differ from other types of pain?
Fibromyalgia pain is widespread, it is located in your muscles and other soft tissues like joints.
Its uniqueness is that this kind of pain affects various sites all over the body.
The mind and body cannot be separated, and so pain is intensified because of the way your brain processes it. If you are stressed or not plays a very important role.
It is important for you to recognize the relationship between stress and pain.
What we all know about life is that it can be very stressful. Sometimes more often than we wished to. You can not get a pill for that. No pill will make stress go away, because stress often doesn’t come from you, but from the environment and actions of other people.
Stress and pain.
Stress is just a part of life!
It is important to know that stress can influence the way you experience pain.
We can differentiate stress. For example, we can see the difference between being stressed by a barking dog, or by having an argument with a family member. But to the body stress is stress, and it will always activate the sympathetic system.
In the case of fibromyalgia pain, stress worsens its condition.
But this is just one aspect of pain – your own stressors. Let’s not forget about other stressors – your life, work, family, friends, finances, hobbies, etc… It all adds up causing a poorer diet, lack of sleep, and relationship issues.
This vicious cycle is very common. I’m sure your partner or yourself experienced that. Pain can easily get out of control!
Fibromyalgia pain can be in the neck, middle, or lower back, arms, legs, shoulders, and hips.

Everyone’s experience with fibromyalgia pain is always different. For example, in the beginning, my wife felt spread pain in only the right side of her body. Later on, it became widespread, affecting both sides.
Some people feel the pain only in certain muscles, other people experience pain all over the body. The quality of such pain also differs from person to person. It may be:
- throbbing
- aching
- burning
- shooting
- stabbing
- soreness
- stiffness
Its intensity can vary and may depend on the time of day, and the activity. Some people have worse pain in the morning, others after they exercise.
In order to diagnose fibromyalgia properly, your doctor – a rheumatologist, will search for 18 pain points on your body that are tender and sensitive to touch.
Diagnosis of fibromyalgia can be difficult because pain is very personal, and your discomfort might not necessarily be the same for someone else. That’s why doctors are meant to check for certain tender points on your body when it comes to diagnosing fibromyalgia.
These 18 points seem like a big number but think of them as 9 pairs. These points tend to be painful when pressed and may spread to other parts of your body.
Let’s list these fibromyalgia tender points once again:
- The back of your neck. If you have fibromyalgia, you may have tender points at the back of your neck.
- Your elbows. Fibromyalgia patients may also feel tenderness on their forearms, near their elbows.
- The front of your neck. The doctor will check your potential fibromyalgia pain at the front of the neck, located above your collarbone, on either side.
- Your pelvis. Hip pain is common and people with fibromyalgia have a tender point near where the buttock muscles curve to join the thighs.
- Lower back. The lower back area is one of the most common body parts to be the source of pain. However, people with fibromyalgia may have pain trigger points at the very top of the buttocks, and right at the bottom of the lower back.
- Knees. While knee pain is common in people with fibromyalgia, the inside of each knee pad may feel tender to the touch.
- Upper back. Tender points are often in places of the body where tendons and muscles meet.
- Shoulders. Additionally, tenderness is in the upper back, but some people with fibromyalgia have tender points just above that, halfway between the edge of the shoulder and the bottom of the neck.
- Your chest. People with fibromyalgia may also have tender points on either side of the sternum, a few inches below the collarbone.
Stress, lack of sleep, and even weather can affect fibromyalgia pain.
Since you are interested in fibromyalgia, I remind you of my “Fibromyalgia for Caring Partners” e-Book, in which 1st chapter is absolutely FREE!
FREE Fibromyalgia e-Book
Fibromyalgia for Caring Men
Treatment of fibromyalgia symptoms…
As you have noticed, it says “treatment of fibromyalgia symptoms” because fibromyalgia cannot be treated directly as an illness. As I mentioned before – you cannot treat the illness, you treat it by targeting its symptoms.
You must focus on all the aspects of your life that are affected by chronic pain, like your work, family, friends, sex, finances, hobbies, etc…
Ideally, as it was in the case of my M, physical therapy works magic in combination with Cognitive-Behavioural Therapy.
Common components of psychological therapy are:
- Pacing of activities.
- Pain & stress physiology.
- Relaxation training.
- Sleep hygiene.
- Identifying stressors.
- Stress management.
- Pain flare-up management.
Fibromyalgia pain affects many aspects of your life, in return – the affected areas of your life impact your pain. It’s a never-ending cycle.
People are told by their doctors, who are wrongly thought by the U.S. Food and Drug Administration (FDA) that treating fibromyalgia can be done with drugs…
But again – you cannot treat chronic pain with the mentality of acute pain treatment. It doesn’t last, you get addicted to drugs, your drug resistance grows, and you increase the risk of overdose.
FDA comes up all the time with fancy names for drugs to get your attention, such as duloxetine (Cymbalta), milnacipran (Savella), or pregabalin (Lyrica).
They work by altering levels of chemicals in your brain and spinal cord that control the transmission of pain signals. I don’t disagree, drugs are fantastic! But they are a great solution for acute pain, not chronic pain!
Relaxation therapies such as CBT, meditation, mindfulness, pilates, yoga, and tai chi are the best way to treat chronic illnesses like fibromyalgia. Also, try to exercise as much and as often as you can. That helps my wife.
Although it might hurt at first, if you stick with light fitness, like walking or bike riding, you will eventually strengthen your muscles and reduce pain.
You can start slowly and gradually increase your intensity, but exercise only when you feel good and ready for it. Don’t push it!
Sleep and overall rest play a big role in fibromyalgia. A lack of sleep can make you feel worse. If you’re struggling to fall asleep, try to avoid or at least limit caffeine and other stimulants (like TV or radio before bed.
Try to go to sleep and wake up at the same time each day. It will allow your body to get into its natural rhythm.
When talking about the checklist for fibromyalgia symptoms, pain is the most obvious. Sometimes it is also the most difficult symptom of fibromyalgia to deal with.
Conclusion on the checklist of fibromyalgia symptoms.
That concludes our checklist for fibromyalgia symptoms and tender points. Remember that these are just some of the more common symptoms associated with fibromyalgia and may not all apply to you personally.
Having a checklist for fibromyalgia symptoms and tender points can help you identify if you may have fibromyalgia or another condition, so you can get the help you need as soon as possible.
To recap, other symptoms like poor concentration, fatigue, depression, or anxiety can also have a big impact on your life. The best thing you can do is to keep track of your symptoms in a diary so you can accurately report them to your doctor. I summarized a checklist for fibromyalgia symptoms.
If you found this article helpful, you can rest assured that this printable checklist for fibromyalgia symptoms won’t disappoint!
Take care!


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…