Fibromyalgia and endometriosis.
My wife, M, suffers from fibromyalgia and endometriosis.
Primarily she was diagnosed with endometriosis and fibromyalgia was just another physiological process that affected her afterward. How common is it to be struggling with multiple medical conditions?
When it comes to chronic illness, many women experience just that.
Endometriosis and fibromyalgia are two distinct medical conditions with no direct causal correlation. Endometriosis involves the abnormal growth of uterine-like tissue outside the uterus, while fibromyalgia is characterized by widespread musculoskeletal pain and fatigue.
While some women may experience both conditions simultaneously, there is no established medical evidence linking the two in terms of causation or shared underlying mechanisms. Both conditions require separate diagnostic and treatment approaches.
Check my video for a closer look, and then scroll down to check the article in more depth…
- Fibromyalgia and Endometriosis
- What are the Gynecological Problems with Fibromyalgia?
- Do Fibromyalgia and Endometriosis Often Coexist?
- Do Fibromyalgia and Endometriosis Impact Each Other?
- When the Body Says No!
- My Wife's Story of Fibromyalgia and Endometriosis
- Trauma and Disease
- Chronic Pain
- A Holistic Approach to Fibromyalgia and Endometriosis
- Conclusion on Fibromyalgia and Endometriosis
Fibromyalgia and Endometriosis
In the endometriosis community, I’ve met many women who suffer from fibromyalgia and endometriosis simultaneously. I spoke to them whilst attending my wife’s endometriosis support group meetings.
I was gobsmacked, by how common fibromyalgia and endometriosis together were affecting so many women.
Quite often women with endometriosis did not know why their pain was spreading beyond the endometriosis areas.
While my wife experienced pain on and off for many years in the past, the pain used to be located in her pelvic area. Over time, the pain has progressed to her legs, and spine, eventually becoming widespread. Her pain became more consistent, eventually becoming a daily struggle, impacting our marriage.

What is Endometriosis?
Endometriosis is a complex and often perplexing condition that affects approximately one in ten women worldwide. This ailment is marked by the growth of tissue resembling the endometrium, which typically lines the uterus, outside of it. The ovaries, fallopian tubes, and tissues lining the pelvis are frequently impacted; in exceptional cases, endometrial tissue may extend beyond pelvic organs.
Despite its appearance outside the womb, this errant tissue mimics typical endometrial behavior: thickening, breaking down and bleeding with every menstrual cycle. However, being displaced from its normal location transforms this natural process into a source of severe pain and discomfort.
There is no way for this blood to exit the body causing pain–often excruciating–inflammation, and eventually potential fertility issues. Symptoms vary widely among those with Endometriosis and severity does not always correspond to pain levels experienced.
One might have visible advancement of the disease yet experience minimal discomfort whereas another may suffer crippling pain despite minor growth. This lack of correlation can complicate diagnosis leading many to live with Endometriosis without being aware.
Endometriosis should not be mistaken or confused with Fibromyalgia – a markedly different condition that presents its own challenges. Fibromyalgia is essentially a disorder characterized by widespread musculoskeletal pain accompanied by fatigue along with sleep, memory and mood issues.
It’s entirely possible for one to exist without the other; Fibromyalgia without Endometriosis or indeed Endometriosis without Fibromyalgia are both common scenarios. While these two conditions are distinctly individual entities each presenting unique symptoms and impacts on life quality, they also share some surprising connections – both apparent and subtle – that hint at possible overlap or coexistence between them.
If you are interested in finding more details about endometriosis, I wrote an “Endo-Tool, Endometriosis for Men” e-Book. You can get a FREE 1st chapter containing 20 pages filled with pure value, such as:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”!
an Endometriosis for Men book

What is Fibromyalgia?
Fibromyalgia is a chronic neurological disorder characterized by widespread musculoskeletal pain, heightened pain response to pressure, fatigue, and psychological distress. It is a condition that permeates the life of the individual who suffers it and can manifest even in people with Endometriosis.
Although it is not directly life-threatening, this malady diminishes the quality of life significantly. The etiology of Fibromyalgia remains elusive and it can occur independently, hence the term “Fibromyalgia without Endometriosis”.
It’s not always associated with another underlying condition like Endometriosis. This disorder confounds medical professionals due to its broad range of symptoms that are often subjective in nature.
The hallmarks of Fibromyalgia include persistent body-wide pain, cognitive difficulties often referred to as “fibro fog,” as well as sleep disturbances. It should be noted that while Fibromyalgia bears some symptomatic resemblance to autoimmune diseases, it does not cause inflammation or damage to tissues or organs.
Unlike autoimmune conditions where there’s an abnormal immune response causing damage, fibromyalgia is thought to stem from abnormalities in how the brain and spinal cord process painful stimuli. In some individuals, symptoms gradually accumulate over time with no single triggering event; in others they may begin after a particular incident such as physical trauma or significant psychological stress.
Some people may also develop Fibromyalgia as part of another disease course like Endometriosis – herein lies its connection with said condition. The complexity intrinsic in diagnosing Fibromyalgia lies within its symptom overlap with other conditions such as rheumatoid arthritis and lupus – diseases which can exist alongside endometriosis without fibromyalgia present.
Additionally, there are no definitive laboratory tests for this disease; diagnosis primarily relies on patient-reported symptoms and a physical examination designed to elicit areas sensitive to light touch known as tender points. Nevertheless, the understanding of Fibromyalgia and its inclusion in medical discussion has evolved significantly over the years, bringing with it hope for those who have experienced this often debilitating disorder.
If you are interested in fibromyalgia, I wrote a “Fibromyalgia for Caring Partners” e-Book, in which 1st chapter is absolutely FREE!
FREE Fibromyalgia e-Book
Fibromyalgia for Caring Men
What are the Gynecological Problems with Fibromyalgia?
Fibromyalgia is a chronic health condition characterized by widespread pain throughout the body, localized areas of tenderness and varying degrees of fatigue, cognitive disturbances and sleep disorders. While Fibromyalgia primarily affects musculoskeletal systems in the body, its effects are not confined to these regions, extending into other domains such as gynecological health.
Fibromyalgia has been associated with various gynecological problems. In many cases, women with Fibromyalgia report gynecological symptoms such as painful periods – medically termed dysmenorrhea – and menorrhagia – a condition defined by heavy or prolonged menstruation.
The basis for this association is still under study; however, it has been proposed that the central sensitization inherent to Fibromyalgia may increase the perception of pain during menstruation. Furthermore, studies have shown an increased prevalence of hysterectomies among women diagnosed with Fibromyalgia.
The reasoning behind this correlation remains uncertain. It could be due to increased levels of pain and discomfort experienced by these women, leading them to opt for more aggressive treatment methods in their search for relief.
It’s vital to note that these difficulties can occur in individuals experiencing Endometriosis without Fibromyalgia as well as those with both conditions; hence attributing them solely to one disease would be misleading. Further complicating the matter is the challenge associated with diagnosing both conditions concurrently due to overlapping symptoms.
A woman suffering from endometriosis may experience similar chronic pelvic pain often observed in women suffering from fibromyalgia causing challenges when attempting proper diagnosis and treatment planning. However intriguingly enough, there are instances where women diagnose fibromyalgia without endometriosis but still present significant gynaecological issues which further emphasizes that Fibromyalgia on its own can lead to substantial female reproductive system disorders.
In essence, while further research is needed to fully comprehend the relationship between Fibromyalgia and gynecological problems, existing studies point towards a correlation that cannot be ignored. Particularly for women who have been diagnosed with fibromyalgia, it is imperative to have regular gynecological evaluations in order to ensure early detection and effective treatment of any potential issues.
Do Fibromyalgia and Endometriosis Often Coexist?
The coexistence of Fibromyalgia and Endometriosis is a medical phenomenon that is now being recognized with increasing frequency in the clinical realm. Recent research suggests that these two conditions often exist concomitantly, thereby presenting a complex clinical picture for both patients and healthcare providers.
The epidemiological data indicate a higher prevalence of fibromyalgia among women with endometriosis as compared to the general population. One might encounter cases of Endometriosis without Fibromyalgia, or vice versa.
However, the concurrence of these two conditions is indeed noteworthy. This frequent simultaneous occurrence has led to an exploration of whether there exist shared etiological factors or if one condition predisposes to the other.
It’s striking how some individuals can manifest symptoms indicative of Fibromyalgia without Endometriosis, while others have prominent endometrial symptoms devoid any fibromyalgic manifestations. A deeper understanding of fibromyalgia and endometriosis aids in comprehending their coexistence better.
Endometriosis involves aberrant growth and presence of endometrial tissue outside the uterine cavity leading to pelvic pain and fertility issues whereas fibromyalgia presents as a syndrome involving widespread musculoskeletal pain accompanied by fatigue, sleep disturbances, memory issues, and mood swings. Uncertainties loom over the precise reasons why individuals with fibromyalgia often tend to have endometriosis too.
Some researchers propose that women diagnosed with one condition may be more vigilant about their health status thus leading to an increased likelihood for diagnosing any additional disease state including either fibromyalgia or endometriosis. Compounding this complexity are instances where symptoms overlap between Fibromyalgia and Endometriosis making definitive diagnosis challenging at times.
For instance, chronic pelvic pain can be a feature both in cases associated solely with either condition and even more so when they coexist. Hence it becomes crucial for clinicians to adopt a comprehensive and nuanced approach towards the management of patients presenting with such medical intricacies.
While cases of Endometriosis without Fibromyalgia or Fibromyalgia without Endometriosis do occur, there is an undeniable coexistence between these two conditions in a significant number of instances. Understanding this interplay further can help in devising more effective therapeutic strategies and improving patient outcomes.
What are Fibromyalgia and Endometriosis Similarities?
The cursory glance at the empiric data of these two seemingly disparate conditions, Fibromyalgia and Endometriosis, reveals striking similarities. Both conditions are chronic and typically cause long-term discomfort with a propensity for flares of acute symptoms. Additionally, both conditions can affect women of any age, but are most common in women of reproductive age and beyond.
It is also noteworthy that both these diseases exhibit gender predominance, with the preponderance occurring in women. Endometriosis without Fibromyalgia can be a debilitating condition, primarily affecting the female reproductive system through growths on organs like ovaries or fallopian tubes; it can cause pelvic pain and fertility problems.
Similarly, Fibromyalgia without Endometriosis is also an impediment to daily living affecting muscles and soft tissues causing widespread musculoskeletal pain accompanied by fatigue, sleep disturbances among other symptoms. Furthermore, both diseases are notoriously nebulous to diagnose due to their overlapping symptomatology with various other ailments; this often leads to delayed diagnoses causing further detriment to patients’ wellbeing.
In endometriosis’s case specifically, symptoms that appear indicative could be attributed to several gynecological or gastrointestinal disorders making diagnosis a formidable challenge for even experienced physicians. The same conundrum exists in fibromyalgia where its diffuse pain could easily be mistaken for arthritis or even depression due to its psychosomatic implications.
The psychological impact of both illnesses should not be underestimated either. Endometriosis and fibromyalgia patients frequently report increased levels of anxiety and depression due to their chronic state of discomfort coupled with uncertain prognoses.
This psychological component further exacerbates physical symptoms creating what many refer as “vicious cycle” where mental distress feeds physical pain which in turn heightens mental anguish. Both endometriosis and fibromyalgia have systemic manifestations beyond their primary targets: female reproductive system for former and musculoskeletal system for latter.
Fatigue, poor sleep quality, cognitive difficulties, sensitivity to touch or pressure are just some of the shared systemic symptoms observed. Though they seem discrete on surface, at their core fibromyalgia and endometriosis share more than just a passing resemblance – they are analogous tales of chronic pain and discomfort that millions of women endure with much resilience and fortitude.
What are Fibromyalgia and Endometriosis Differences?
While fibromyalgia and endometriosis may overlap in certain aspects such as their chronicity and their impact on a patient’s quality of life, it is paramount to understand that they are indeed distinct conditions with unique distinguishing traits. To begin, endometriosis is fundamentally an inflammatory condition that manifests predominantly in the pelvic region. This disorder arises when tissues similar to the lining of the uterus grow outside of it, often causing severe abdominal pain and other complications.
Importantly, these symptoms fluctuate with hormonal changes throughout a woman’s menstrual cycle. Endometriosis is routinely confirmed through surgical procedures like laparoscopy that offer direct visualization of endometrial implants outside the uterus.
This characteristic makes it distinctly different from fibromyalgia which has no specific diagnostic test. Fibromyalgia, on the other hand, is primarily a neurologic condition characterized by widespread musculoskeletal pain accompanied by fatigue, sleep disturbances, memory issues and mood swings.
Unlike endometriosis which concentrates its effects in one general area (the pelvis), fibromyalgia’s hallmark symptom of pain can be experienced throughout various parts of the body. Fibromyalgia also does not have visible physical signs or abnormalities that can be detected through traditional medical imaging or laboratory tests.
Additionally, while both conditions can cause considerable discomfort and distress to patients, their treatments vary significantly because they target different mechanisms contributing to each disease. Endometriosis is commonly treated using hormonal therapy or surgery with the aim to control aberrant endometrial growths causing discomfort; whereas for fibromyalgia without endometriosis treatment often consists of medications designed to manage pain and improve sleep alongside lifestyle modifications.
Moreover, another point of divergence between these two conditions pertains to their gender predominance. While both men and women can develop fibromyalgia – albeit at different rates – endometriosis exclusively affects individuals assigned female at birth, as it is fundamentally tied to the presence of a uterus and menstrual cycle.
This crucial difference highlights how fibromyalgia without endometriosis can impact a wider range of individuals across the gender spectrum. While fibromyalgia and endometriosis may evoke similar experiences in pain and distress for those suffering from them, they are indeed distinct conditions.
They should be recognized for their unique characteristics, to ensure that individuals receive the appropriate diagnosis and treatment. Despite possible overlaps in symptoms or co-occurrence in some patients, it is critical we maintain clear distinctions between these two conditions in our understanding and approach.
Do Fibromyalgia and Endometriosis Impact Each Other?
It is vitally important to recognize the interconnected nature of Fibromyalgia and Endometriosis, especially as it pertains to their potential exacerbating effects on one another. While each condition can indeed exist independently, in many instances, the two afflictions coexist within a single individual, thereby underscoring an unmistakeable mutual impact. Endometriosis is a condition where cells akin to those lining the uterus grow outside it, creating a series of complications including chronic pain.
Coincidentally, Fibromyalgia is distinguished by its exceptional body tenderness and unrelenting fatigue amongst other symptoms. The presence of these two conditions simultaneously undeniably amplifies the overall discomfort faced by patients.
Fibromyalgia without Endometriosis tends to display rather distinct characteristics compared to when it coexists with Endometriosis. In isolation, Fibromyalgia predominantly presents widespread musculoskeletal pain which often disrupts sleep patterns and cognitive function.
However, when coupled with Endometriosis, patients experience an amplified level of discomfort due to additional pelvic pain and potential gastrointestinal issues. Similarly noteworthy are instances of Endometriosis without Fibromyalgia.
Patients grappling solely with Endometriosis primarily suffer from chronic pelvic pain consistent with their menstrual cycle alongside potential fertility concerns. Nonetheless, this level of distress can escalate dramatically when compound by Fibromyalgia’s overarching fatigue and tender points throughout the body.
Ultimately though empirical studies are still being conducted on this interplay between Endometriosis and Fibromyalgia; there’s irrefutable evidence that these disorders intensify each other’s symptoms significantly when present concurrently within an individual. This mutual enhancement prolongs the healing process and hampers timely recovery leading to increased suffering for patients affected by both conditions together compared individually.
When the Body Says No!
According to Dr. Gabor Maté, who I admire immensely, chronic illness and chronic pain originate from childhood trauma. That also applies to fibromyalgia and endometriosis.
Gabor wrote the book “When the Body Says No”, which my wife has read and loved. It helped her understand that who gets sick and who doesn’t isn’t accidental!
Chronic illness isn’t a random event, so weren’t my wife’s fibromyalgia and endometriosis.
Occasionally we can explain the cause. For instance, lung cancer occurs because of a lifestyle that a person chooses – smoking.
But when it comes to chronic illnesses like fibromyalgia and endometriosis, they are always rooted in childhood.
Both diseases are physiological processes, and we know from science that the mind and body can’t be separated.
I always say that physical and mental health, both impact one another, and both should never be seen as separate.
Doctors should look at the patient as a whole, not accuse of being anxious or depressed when in reality people suffer from invisible to others but real, chronic pain.
People who suffer from fibromyalgia and endometriosis experienced a lot of stress in the past.
This stress usually begins in childhood. That wasn’t only what my wife experienced, but every single woman suffering from fibromyalgia and endometriosis that I have spoken to.
If you suffer from either disease or even both – fibromyalgia and endometriosis, I urge you to read the book “When the Body Says No – The Cost of Hidden Stress” written by Dr. Gabor Maté.
His book explores the role of the mind-body link in various chronic conditions. It is about the body saying no to stresses in life that people haven’t dealt with when needed to.
This book asks questions such as:
- How much your loved ones stress you take on?
- How much of a people pleaser are you?
- How nice are you to people no matter how you feel?
- How much do you take on the problems of other people and ignore your own?
- How well do you know yourself?
- Do you treat yourself well?
All these questions perfectly apply 100% to my wife! I wonder if you can relate to them too?
It all started when M wanted to say no but she was afraid of what people were going to say, or she was afraid of rejection, of not being loved, or even of not being a good person.
If you engage with these questions as my wife did, your body will respond very positively.
I cannot recommend this book enough!
Dr. Gabor Maté explores in the book the role of the mind-body link in conditions and diseases such as arthritis, cancer, diabetes, heart disease, irritable bowel syndrome, multiple sclerosis, even fibromyalgia, and endometriosis.
He is a retired physician who, after 20 years of family practice and palliative care experience, worked for over a decade with patients challenged by drug addiction and mental illness.
My Wife’s Story of Fibromyalgia and Endometriosis
Fibromyalgia and endometriosis that my wife suffers from, both originated in her childhood.
She went through hell when she was little. Her father brought a lot of trauma into her life. I won’t go into the details because it is not my place to say.
However, as a child, it made her frightened and extremely anxious about what he was going to do. M worried about her mum being mistreated by her father and couldn’t focus at school.
She felt very isolated and other kids noticed that. They began to bully her for years to come.
There was a point when she couldn’t stand it anymore and left school to have private tuition at home.
Doctors put her on Prozac at the age of 15 and left her on antidepressants for the next 18 years. In my opinion, wrongly.
Instead of focusing on the causes of her stressful childhood, it was easier for them to put her on Prozac. That is extremely common these days, which I strongly disagree with.
As a teenager, she found a passion for dancing to become a professional dancer in the future.
However, being a talented and better dancer than other girls, once again, she was bullied for being “different”.
More trauma, more stress, more problems… She got ill with anorexia and additionally fell into depression. Aside from that M developed Obsessive Compulsive Disorder due to her being a perfectionist.
In her early adolescence, she had a few relationships with men, who weren’t so nice to her. One of them was a drug addict and a bully.
Eventually, she met a nice guy who also was a dancer, and who treated her really well, but after 7 years of relationship, he told her that he did not see the future with her.
During 35 years of her life, M experienced a lot of trauma and was betrayed by people, whom she trusted the most.
But as she was on the verge of giving up, she met me. Mr nice guy!
She fell in love and I became the one for her.
M trusted me, I was the first man who never disappointed her. Furthermore – I cared for her, gave her the love and warmth she needed.
M finally found security and felt wanted, and needed.
We got married in the spring of 2012 becoming the happiest couple on earth, both sharing our passion for dancing, and traveling. We had everything we needed.
On our wedding day, my wife told me that she came to Prozac.
She did very well despite her doctors never keeping an eye on her antidepressants for 18 years. She came off them on her own, gradually over a period of 8 months.
Her life seemed to have changed. But the happiness didn’t last long…
Trauma and Disease
Women with both fibromyalgia and endometriosis have a higher risk of having other autoimmune diseases such as IBS and chronic fatigue syndrome, anxiety, or depression as well as more hospitalizations.
As it happens, my wife so far experienced all of them, as well, as Obsessive-Compulsive Disorder. She has other gastric problems like acid reflux and heartburn, she also suffers from Iron and Magnesium deficiency.
Women who were diagnosed with endometriosis after surgery reported a high prevalence of fibromyalgia. That was the case with my wife. The trauma of endometriosis brought fibromyalgia.
So, are endometriosis and fibromyalgia related?
According to research from Southwest Spine and Pain Center, “women with endometriosis were twice as likely to have fibromyalgia than those who did not have the condition.
Moreover, 31% of women diagnosed with endometriosis had also been diagnosed with fibromyalgia. Although researchers are unsure as to why both conditions are linked, it is clear fibromyalgia and endometriosis do have some kind of relationship.”

My wife has deep infiltrating endometriosis and there is a prevalence of fibromyalgia amongst women with deep infiltrating endometriosis.
Ever since she began to experience various pain flare-ups. She’s actually experiencing a stabbing endometriosis pain as we speak!
It’s hard to talk about pain flares when you don’t experience them yourself. I have seen my M in pain enough times to know, that these flare-ups can sometimes overlap.
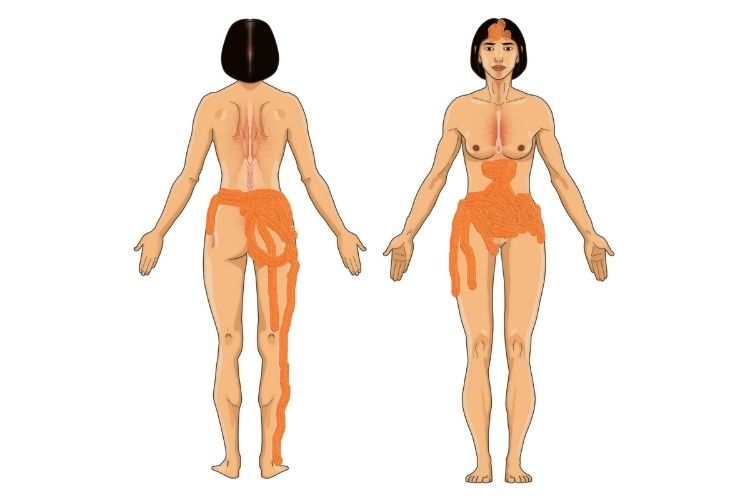
There are days, especially around her ovulation or period itself, when M experiences stabbing pains which are usually localized in her lower stomach and pelvic area, going down to her legs.
Other times, the pain takes a different form and spreads all over her body. It can be either – sharp, burning in sensation, feel like a dull muscular ache, can be numbing, or her skin is very sensitive to touch.
But there are times when the pain takes a mixed form, coming from both – fibromyalgia and endometriosis.
These are the days when my wife literally climbs the walls in pain.
M used to get frustrated trying to explain her pain, my lack of understanding wasn’t helpful either. After all, I’m a man, and I don’t experience what she’s going through.
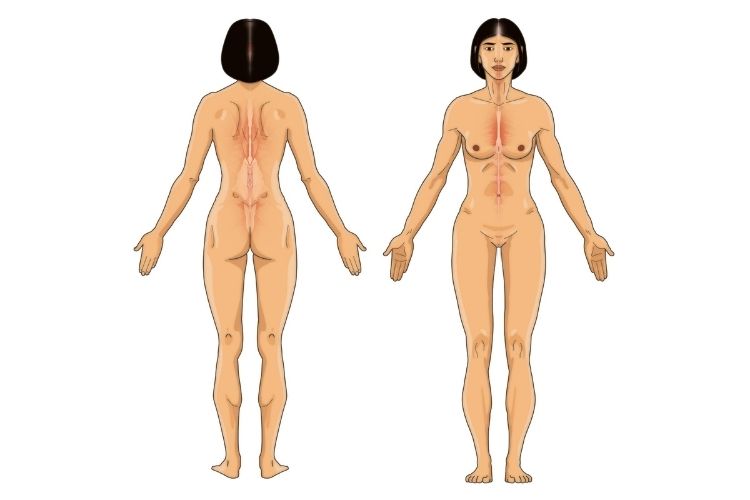
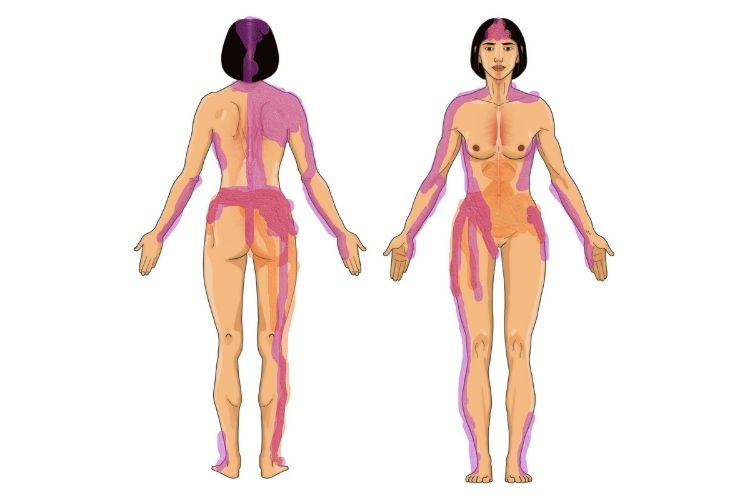
One day, I came up with an idea and created a body map on which my wife could draw the pain that she felt.
To illustrate that I will provide you with her own drawings. The first one was blank and ready to be filled:
Second one M marked with endometriosis pain:
The third one resembled fibromyalgia pain:
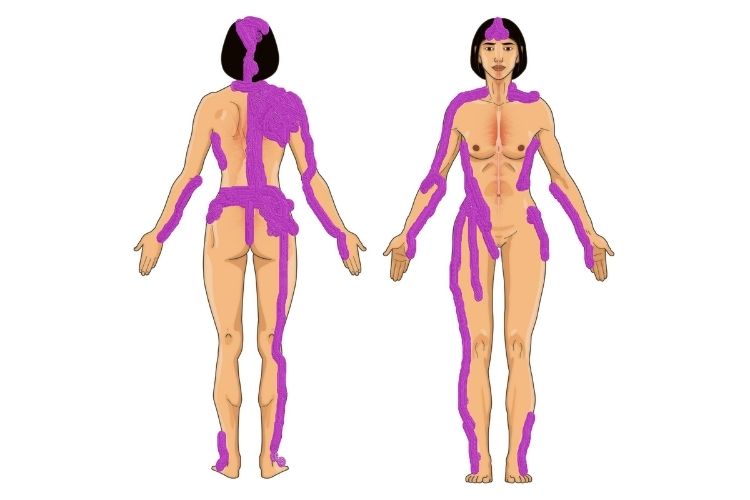
Lastly, I combined both overlapping each other to reveal how much pain my wife was really going through:
Chronic Pain
Chronic pain is the main symptom of most chronic illnesses, especially fibromyalgia and endometriosis.
Chronic diseases don’t strike people for no reason. These diseases are not mysterious and they don’t just come from nowhere. There are always some patterns that can be identified.
My wife was puzzled about why she got endometriosis. There was no one in her family who experienced it before.
We learned over time that her fibromyalgia was the reaction to endometriosis.
One in ten women of reproductive age suffers from endometriosis. The problem is that not all of them know it. Many women haven’t even heard of endometriosis.
But when you have a diagnosis of fibromyalgia, this complicates things even further. Any new pain is doubled because of endometriosis if there is a day when they overlap one another.
Endometriosis directly irritates nerves creating an inflammatory response, which has wide-ranging effects on your body. As the endometriosis tissue breaks down and bleeds, your body creates scars called adhesions, which can stick your pelvic organs together.
It can also infiltrate organs like the bowel (my wife’s case) and the bladder, causing even more problems. M goes to the toilet often at night because scars caused by adhesions irritate her bladder.
There is a similarity between fibromyalgia and endometriosis, because women with fibromyalgia, also deal with a lot more pain and fatigue during their periods, and that is always the case for my wife.
People wrongly think that endometriosis symptoms can be managed by hormonal contraceptives. This is not always the case, it may give you some form of relief, but it won’t treat the disease! Unfortunately, it doesn’t work for all women and may even stop working as endometriosis progresses.
Similarly, people wrongly think that fibromyalgia pain can be managed with painkillers. Again, that is not the case. You cannot treat chronic pain with the mindset of acute pain management.
I explain this very well in detail in my acute vs chronic pain article.
Emotions can play a role in making a person susceptible to diseases. Chronic stress sensitizes the immune system, which becomes overly reactive to any number of triggers.
The importance of positive social and personal relationships in modulating stress isn’t recognized. But my relationship of 13 years with a chronically ill wife thought me precisely that!
A Holistic Approach to Fibromyalgia and Endometriosis
M’s symptoms of fibromyalgia and endometriosis improve whenever she’s around me. I never cause her stress, furthermore, I support her on every level, physically and emotionally.
Such a healthy and safe environment improves my wife’s pain. But whenever she thinks of going back to work on Monday, which is one of the triggers, her symptoms begin to arise.
My wife is happily married, and she’s lucky because the study shows that those who are unhappily married and suppress their feelings are for times more likely to die. It sounds drastic but I give you these facts to stress the importance of not holding your emotions.
When suppressing your emotions, your body eventually responds. This is also the case of fibromyalgia and endometriosis.
You cannot separate the mind and body. Your body will always react to your emotions. Positive emotions make the immune system stronger, stress switches off your immune system.
Because at any one time, cells, in other words, your entire body, can be either in defensive mode or growth mode but never both.
If you’re stressed, your body switches to either, fight or flight mode. What happens then is that blood rushes to your limbs away from your gut in case you have to escape or fight.
When your gut is switched off, it can’t fight bacteria or viruses. Your body becomes an easy target. This is when you catch flu, not due to “lack of vitamin C” – there’s no evidence of the latter.
So, stress is not good because it makes your body vulnerable.
This is why the importance of having the right support of a loved one is crucial. Fibromyalgia and endometriosis react to how you feel.
Ask yourself this – whenever you go to the doctor in search of a diagnosis, do they ever ask about your childhood, relationships, marriage? Most probably the answer is no. Instead, they tell you that you have an illness and there’s nothing you can do.
They always assume that you are anxious or depressed. They don’t even ask you why do you feel stressed, and most of the time is the opposite – illness, and pain is the cause of stress.
But most doctors don’t see that. They just try and give you pill after pill. That’s all they do.
They don’t ask about the life factors that contribute to your fibromyalgia and endometriosis.
But it is important to treat these chronic illnesses by targeting the areas of life that are affected by illness and pain such as work, family, relationships, sex life, social life…
The management of fibromyalgia and endometriosis has the same approach as for any other chronic conditions which lack a cure.
It’s about improving the quality of life and functioning.
Chronic pain management requires:
- Medical optimization (CBD for example).
- Physical reconditioning (rehabilitation).
- Behavioral, lifestyle modification (pain psychologist).
- Helping people become more aware of what these factors are, and how they influence pain, is a big part of behavioral and lifestyle modification.
People often think that they need to belong to only one of these categories, but in order to effectively treat chronic pain, you need to consider all the factors.
Fibromyalgia and endometriosis affect many aspects of your life:
- Family, friends.
- Work, school.
- Sports, leisure.
- Self-care.
- Vacations, hobbies.
- Socializing, entertainment.
- Cooking, cleaning, errands.
Neglect of the management of these factors, or the wrong, acute approach to managing chronic pain, will impact you not only physically, but also mentally and financially, and the vicious cycle will continue…
The suffering of fibromyalgia and endometriosis pain doesn’t build character, it breaks it!
This is why it is vital to have the right support from your loved ones. But what not many websites and blogs dedicated to fibromyalgia and endometriosis tell you is the impact these illnesses have on the caregivers.
Unfortunately, we – supporters of those who suffer, are always forgotten!
No one talks about our struggles, and yet, as it was in my experience, my wife’s fibromyalgia and endometriosis not only affected her but also me – her husband.
I’ve written an article on the subject of how to cope with a chronically ill spouse.
I summarized it at the beginning in one sentence, that in order to a chronically ill loved one, you need to focus on changing yourself rather than “fixing” your partner’s health.
My wife tried to take her own life on a few occasions, she even asked me to divorce her five times.
M did all this because of the guilt she felt that I wasn’t fulfilling my life being with her. She loved me so much, that she was ready to make the ultimate sacrifice. Asking me to divorce her wasn’t easy either.
Life can be cruel for those who suffer from fibromyalgia and endometriosis, but my life wasn’t sunshine and puppy cuddles either. I went through a lot, I sacrificed my own time, my passions, and sometimes even my job in order to help her go through this.
So, chronic illness affects more than one person and those who support their loved ones should never be forgotten. Our mental health matters!
I hope you found this article informative. I honestly cannot recommend the book “When the Body Says No” enough! It is going to add a lot of value to your life.
Conclusion on Fibromyalgia and Endometriosis
In the vast and complex field of medical science, endometriosis and fibromyalgia often present as elusive enigmas. Notwithstanding their intricate nature, strides are being made continuously to understand them better and develop effective treatment strategies.
The myriad of symptoms that accompany these conditions often intersect, leading to a more arduous diagnostic process. It is unsurprising, then, that many patients with fibromyalgia may have undiagnosed endometriosis or vice versa.
It is essential to bear in mind that one can have fibromyalgia without endometriosis. Similarly, there are those who grapple with endometriosis but do not suffer from fibromyalgia.
Each condition bears its own weight of complications and discomforts. Yet the interlinking complexities undoubtedly compound when these two conditions occur concurrently.
To put it succinctly, while both conditions manifest distinct pathological features, similarities exist in the form of chronic pain and fatigue — hallmarks that make living with either condition a significant challenge. Moreover, they both impact the quality of life, causing physical limitations and socio-psychological burdens for those afflicted.
On the bright side,and underscoring an optimistic note in this otherwise austere discourse – our understanding of these two conditions has expanded remarkably in recent years. This accelerated knowledge helps pave the way for improved diagnostic accuracy and therapeutic options for patients with either or both conditions.
Despite the burdensome nature of living with endometriosis or fibromyalgia — let alone both — there is cause for optimism as our understanding continues to grow steadily about these complex biological phenomena. As long as research progresses unabated into their mechanisms and potential treatments — hope persists on the horizon for those grappling daily with their symptoms.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men...
